Abstract
Summary
We compared the distribution of vertebral fractures in adults and children and found that fractures occurred in different locations in the two age groups. This likely relates to the different shape of the immature spine.
Introduction
We hypothesized that the anatomical distribution of vertebral fractures (VF) would be different in children compared to adults.
Methods
We compared the distribution of VF defined using the Genant semi-quantitative method (GSQ method) in adults (N = 221; 545 fractures) and in children early in the course of glucocorticoid therapy (N = 44; 94 fractures).
Results
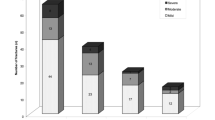
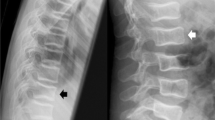
The average age in the adult cohort was 62.9 years (standard deviation (SD), 13.4 years), 26% was male, the mean lumbar spine Z-score was −1.0 (SD, 1.5), and the corresponding T-score was −2.4 (SD, 1.4). The pediatric cohort median age was 7.7 years (range, 2.1–16.6 years), the mean lumbar spine Z-score was −1.7 (SD, 1.5), 52% was male, and disease categories were acute lymphoblastic leukemia (66%), rheumatological conditions (21%), and nephrotic syndrome (14%). The VF distribution was biphasic in both populations, but the peaks differed in location. In adults, the peaks were at T7/T8 and at T12/L1. In children, the focus was higher in the thoracic spine, at T6/T7, and lower in the lumbar spine, at L1/L2. When children were assessed in two age-defined sub-groups, a biphasic VF distribution was seen in both, but the upward shift of the thoracic focus to T6 was observed only in the older group, with the highest rates of fracture present between ages 7 and 10 years.
Conclusions
These results suggest that the anatomical distribution of VF differs between children and adults, perhaps relating to the different shape of the immature spine, notably the changing ratio of kyphosis to lordosis.





Similar content being viewed by others
References
Silva MJ (2007) Biomechanics of osteoporotic fractures. Injury 38S3:S69–S76
Zebaze R, Maalouf G, Maalouf N, Seeman E (2004) Loss of regularity in the curvature of the thoracolumbar spine: a measure of structural failure. J Bone Miner Res 19:1099–1104
Legaye J, Duval-Beaupere G (2008) Gravitational forces and sagittal shape of the spine. Clinical estimation of their relations. Int Orthop 32:809–816
Legaye J, Duval-Beaupere G (2005) Sagittal plane alignment of the spine and gravity. A radiological and clinical evaluation. Acta Orthop Belg 71:213–220
Cil A, Yazici M, Uzumcugil A et al (2004) The evolution of sagittal segmental alignment of the spine during childhood. Spine 30:93–100
Lunt M, O’Neill TW, Felsenberg D et al (2003) Characteristics of a prevalent vertebral deformity predict subsequent vertebral fracture: results from the European Prospective Osteoporosis Study (EPOS). Bone 33:505–513
Healy JH, Lane JM (1985) Structural scoliosis in osteoporotic women. Clinical Orthop Relat Res 195:216–223
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148
Chapurlat RD, Duboeuf F, Marion-Audibert HO, Kalpakcioglu B, Mitlak BH, Delmas PD (2006) Effectiveness of instant vertebral assessment to detect prevalent vertebral fracture. Osteoporos Int 17:1189–1195
Fechtenbaum J, Cropet C, Kolta S, Verdoncq B, Orcel P, Roux C (2005) Reporting of vertebral fracture on spine X-rays. Osteoporos Int 16:1823–1826
Fuerst T, Wu C, Genant HK et al (2009) Evaluation of vertebral fracture assessment by dual X-ray absorptiometry in a multicenter setting. Osteoporos Int 20:1199–1205
Genant HK, Jergas M, Palermo L et al (1996) Comparison of semiquantitative visual and quantitative morphometric assessment of prevalent and incident vertebral fractures in osteoporosis. J Bone Miner Res 11:984–996
Leidig-Bruckner G, Genant HK, Minne HW et al (1994) Comparison of a semiquantitative and a quantitative method for assessing vertebral fractures in osteoporosis. Osteoporos Int 4:154–161
Rea JA, Li J, Blake GM, Steiger P, Genant HK, Fogelman I (2000) Visual assessment of vertebral deformity by X-ray absorptiometry: a highly predictive method to exclude vertebral deformity. Osteoporos Int 11:660–668
Vallarta-Ast N, Krueger D, Wrase C, Agrawal S, Binkley N (2007) An evaluation of densitometric vertebral fracture assessment in men. Osteoporos Int 18:1405–1410
Wu CY, Li J, Jergas M, Genant HK (1995) Comparison of semiquantitative and quantitative techniques for the assessment of prevalent and incident vertebral fractures. Osteoporos Int 5:354–370
Huber AM, Gaboury I, Cabral DA et al (2010) Prevalent vertebral fractures among children initiating glucocorticoid therapy for the treatment of rheumatic disorders. Arthritis Care Res 62:516–528
Halton J, Gaboury I, Grant R et al (2009) Advanced vertebral fracture among newly diagnosed children with acute lymphoblastic leukemia: results of the Canadian Steroid-associated Osteoporosis in the Pediatric Population (STOPP) Research Program. J Bone Miner Res 24:1326–1334
Feber J, Gaboury I, Ni A et al (2011) Skeletal findings in children initiating glucocorticoids for the treatment of nephrotic syndrome. Osteoporos Int (in press)
Willner S, Johnson B (1983) Thoracic kyphosis and lumbar lordosis during the growth period in children. Acta Paediatr Scand 72:873–878
Singer KP, Jones TJ, Breidahl PD (1990) A comparison of radiographic and computer-assisted measurements of thoracic and thoracolumbar sagittal curvature. Skeletal Radiol 19:21–26
Nissensen M (1995) Spinal posture during pubertal growth. Acta Paediatr 84:308–312
Siminoski K, Warshawski RS, Jen H, Lee K (2006) The accuracy of historical height loss for the detection of vertebral fractures in postmenopausal women. Osteoporos Int 17:290–296
Ogden CL, Kuczmarski RJ, Flegal KM et al (2000) Centers for Disease Control and Prevention 2000 growth charts for the United States: improvements to the 1977 National Center for Health Statistics version. Pediatrics 109:45–60
Yuan HA, Brown CW, Phillips FM (2004) Osteoporotic spinal deformity. A biomechanical rationale for the clinical consequences and treatment of vertebral body compression fractures. J Spinal Disord Tech 17:236–242
Myers ER, Wilson SE (1997) Biomechanics of osteoporosis and vertebral fracture. Spine 22(Suppl 2):25S–31S
Briggs AM, Greig AM, Wark JD (2007) The vertebral fracture cascade in osteoporosis: a review of aetiopathogenesis. Osteoporos Int 18:575–584
Andersson GBJ (1992) Biomechanics of the spine. In: Kirkadldy-Willis WH, Burton CV (eds) Managing low back pain, 3rd edn. Churchill Livingstone, New York, pp 27–37
Davison KS, Siminoski K, Adachi JD et al (2006) Bone strength the whole is greater than the sum of its part. Semin Arthritis Rheum 36:22–31
Trout AT, Kallmes DF, Layton KF, Thielen KR, Hentz JG (2006) Vertebral endplate fracture: an indicator of the abnormal forces generated in the spine after vertebroplasty. J Bone Miner Res 21:1797–1802
Nakhla M, Scuccimarri R, Duffy KN et al (2009) Prevalence of vertebral fractures in children with chronic rheumatic disease at risk for osteopenia. J Pediatr 154:438–443
Varonos S, Ansell BM, Reeve J (1987) Vertebral collapse in juvenile chronic arthritis: its relationship with glucocorticoid therapy. Calcif Tissue Int 41:75–78
Cooper C, Atkinson EJ, O’Fallon WM, Melton LJ (1992) Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985–1989. J Bone Miner Res 7:221–227
Reilly CW (2007) Pediatric spine trauma. J Bone Joint Surg 89-A(Suppl 1):98–107
Hegenbarth R, Ebel KD (1976) Roentgen findings in fractures of the vertebral column in childhood. Pediat Radiol 5:34–39
Leonard M, Sproule J, McCormack D (2007) Paediatric spinal trauma and associated injuries. Injury 38:188–193
Ferrar L, Jiang G, Clowes JA, Peel NF, Eastell R (2008) Comparison of densitometric and radiographic vertebral fracture assessment using the algorithm-based qualitative (ABQ) method in postmenopausal women at low and high risk of fracture. J Bone Miner Res 23:103–111
Ismail AA, Cooper C, Falsenberg D et al (1999) Number and type of vertebral deformities: epidemiological characteristics and relation to back pain and height loss. Osteoporos Int 9:206–213
Siris ES, Genant HK, Laster AJ, Chen P, Misurski DA, Krege JH (2007) Enhanced prediction of fracture risk combining vertebral fracture status and BMD. Osteoporos Int 18:761–770
Delmas PD, Genant HK, Crans GG et al (2003) Severity of prevalent vertebral fractures and the risk of subsequent vertebral and non-vertebral fractures: results from the MORE trial. Bone 33:522–532
Tanko LB, Christiansen C, Cox DA, Geiger MJ, McNabb MA, Cummings SR (2005) Relationship between osteoporosis and cardiovascular disease in postmenopausal women. J Bone Miner Res 20:1912–1920
Ferrar L, Jiang G, Cawthon PM et al (2007) Identification of vertebral fracture and non-osteoporotic short vertebral height in men: the MrOS study. J Bone Miner Res 22:1434–1441
Gaca AM, Barnhart HX, Bisset GS (2010) Evaluation of wedging of lower thoracic and upper lumbar vertebral bodies in the pediatric population. Am J Roentgenol 194:516–520
Goh S, Price RI, Song S, Davis S, Singer KP (2000) Magnetic resonance-based vertebral morphometry of the thoracic spine: age, gender and level-specific influences. Clin Biomech 15:417–425
Natsui K, Tanaka K, Suda M et al (2006) High-dose glucocorticoid treatment induces rapid loss of trabecular bone mineral density and lean body mass. Osteoporos Int 17:105–108
Acknowledgments
The Canadian STOPP Consortium would like to thank the children and their families who participated in the study and without whom the STOPP research program would not have been possible.
STOPP would also like to thank the following:
The research associates who managed the study at the Children’s Hospital of Eastern Ontario: Steve Anderson (project management), Victor Konji (project management), Catherine Riddell (project management), Maya Scharke (data analysis, database management), Elizabeth Sykes (project management), Monica Tomiak (statistical analysis).
The research associates who took care of the patients: Claude Belleville, Ronda Blasco, Erika Bloomfield, Dan Catte, Heather Cosgrove, Susan Docherty-Skippen, Diane Laforte, Maritza Laprise, Josie MacLennan, Natacha Gaulin Marion, Leila MacBean, Amanda Mullins, Michele Petrovic, Eileen Pyra, Mala Ramu, Angelyne Sarmiento, Terry Viczko, and Aleasha Warner.
The research nurses and support staff from the various Divisions of Nephrology, Oncology, Rheumatology and Radiology who have contributed to the care of the children enrolled in the study.
The STeroid-associated Osteoporosis in the Pediatric Population (STOPP) Consortium:
Alberta Children’s Hospital, Calgary, Canada: Reinhard Kloiber, Victor Lewis, Julian Midgley, Paivi Miettunen, David Stephure; British Columbia Children’s Hospital, Vancouver, Canada: David Cabral, David B. Dix, Kristin Houghton, Helen R. Nadel; British Columbia Women’s Hospital and Health Sciences Center, Vancouver, Canada: Brian C. Lentle; Brock University, St. Catharines, Canada: John Hay; Children’s Hospital of Eastern Ontario, Ottawa, Canada: Janusz Feber, Jacqueline Halton, Roman Jurencak, MaryAnn Matzinger, Johannes Roth, Nazih Shenouda, Leanne M. Ward; IWK Health Center, Halifax, Canada: Elizabeth Cummings, Conrad Fernandez, Adam M. Huber, Bianca Lang, Kathy O’Brien; McMaster Children’s Hospital, Hamilton, Canada: Stephanie Atkinson, Steve Arora, Ronald Barr, Craig Coblentz, Peter B. Dent, Maggie Larche, Colin Webber; Montreal Children’s Hospital, Montreal, Canada: Sharon Abish, Lorraine Bell, Celia Rodd, Rosie Scuccimarri; Ottawa Hospital Research Institute, Ottawa, Canada: David Moher, Tim Ramsay; Shriners Hospital for Children, Montreal, Canada: Francis Glorieux, Frank Rauch; Ste. Justine Hospital, Montreal, Canada: Nathalie Alos, Caroline Laverdiere, Josee Dubois, Veronique Phan, Claire Saint-Cyr; Stollery Children’s Hospital, Edmonton, Canada: Robert Couch, Janet Ellsworth, Claire LeBlanc, Maury Pinsk, Kerry Siminoski, Beverly Wilson; Toronto Hospital for Sick Children, Toronto, Canada: Martin Charron, Ronald Grant, Diane Hebert; Universite de Sherbrooke, Sherbrooke, Canada: Isabelle Gaboury; University of Western Ontario, London, Canada: Elizabeth Cairney, Cheril Clarson, Guido Filler, Joanne Grimmer, Keith Sparrow, Robert Stein; Winnipeg Children’s Hospital, Winnipeg, Canada: Tom Blydt-Hansen, Sara Israels, Kiem Oen, Martin Reed, Shayne Taback
Conflicts of interest
H. Nadel received an honorarium from Siemens Canada for speaking at a radiology symposium. None of the other authors have any disclosures.
Funding
The primary funding source of this study was from The Canadian Institutes of Health Research. Additional funding sources were from The Canadian Child Health Clinician Scientist Program, The Children’s Hospital of Eastern Ontario Research Institute, and Women and Children’s Health Research Institute, University of Alberta.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Siminoski, K., Lee, KC., Jen, H. et al. Anatomical distribution of vertebral fractures: comparison of pediatric and adult spines. Osteoporos Int 23, 1999–2008 (2012). https://doi.org/10.1007/s00198-011-1837-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-011-1837-1