Abstract
Summary
In the Study of Osteoporotic Fractures (SOF), 18.5 % of incident hip fractures identified in Medicare Fee-for-Service claims data were not reported to or confirmed by the cohort. Cognitive impairment was a modest risk factor for false-negative hip fracture ascertainment via self-report.
Introduction
Prospective cohort studies of fractures that rely on participant self-report to be the initial signal of an incident fracture could be prone to bias if a significant proportion of fractures are not self-reported.
Methods
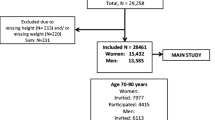
We used data from the SOF merged with Medicare Fee-for-Service claims data to estimate the proportion of participants who had an incident hip fracture identified in Medicare claims that was either not self-reported or confirmed (by review of radiographic reports) in SOF.
Results
Between 1/1/1991 and 12/31/2007, 647 SOF participants had a hip fracture identified in Medicare claims, but 120 (18.5 %) were either not reported to or confirmed by the cohort. False-negative hip fracture ascertainment was associated with a reduced modified Mini-Mental State Exam (MMSE) score (odds ratio 1.31 per SD decrease, 95 % C.I. 1.06–1.63). Point estimates of associations of predictors of incident hip fracture were changed minimally when the misclassification of incident hip fracture status was corrected with use of claims data.
Conclusions
A substantial minority of incident hip fractures were not reported to or confirmed in the SOF. Cognitive impairment was modestly associated with false-negative hip fracture ascertainment. While there was no evidence to suggest that misclassification of incident hip fracture status resulted in biased associations of potential predictors with hip fracture in this study, false-negative incident fracture ascertainment in smaller cohort studies with limited power may increase the risk of type 2 error (not finding significant associations of predictors with incident fractures).


Similar content being viewed by others
References
Bergmann MM, Byers T, Freedman DS et al (1998) Validity of self-reported diagnoses leading to hospitalization: a comparison of self-reports with hospital records in a prospective study of American adults. Am J Epidemiol 147(10):969–977
Chen Z, Kooperberg C, Pettinger MB et al (2004) Validity of self-report for fractures among a multiethnic cohort of postmenopausal women: results from the Women's Health Initiative observational study and clinical trials. Menopause 11(3):264–274
Honkanen K, Honkanen R, Heikkinen L et al (1999) Validity of self-reports of fractures in perimenopausal women. Am J Epidemiol 150(5):511–516
Ismail AA, O'Neill TW, Cockerill W et al (2000) Validity of self-report of fractures: results from a prospective study in men and women across Europe. EPOS Study Group. European Prospective Osteoporosis Study Group. Osteoporos Int 11(3):248–254
Beard CM, Melton LJ 3rd, Cedel SL et al (1990) Ascertainment of risk factors for osteoporosis: comparison of interview data with medical record review. J Bone Miner Res 5(7):691–699
Ivers RQ, Cumming RG, Mitchell P et al (2002) The accuracy of self-reported fractures in older people. J Clin Epidemiol 55(5):452–457
Hundrup YA, Hoidrup S, Obel EB et al (2004) The validity of self-reported fractures among Danish female nurses: comparison with fractures registered in the Danish National Hospital Register. Scand J Public Health 32(2):136–143
Siggeirsdottir K, Aspelund T, Sigurdsson G et al (2007) Inaccuracy in self-report of fractures may underestimate association with health outcomes when compared with medical record based fracture registry. Eur J Epidemiol 22(9):631–639
Virnig B, Durham SB, Folsom AR et al (2010) Linking the Iowa Women's Health Study cohort to Medicare data: linkage results and application to hip fracture. Am J Epidemiol 172(3):327–333
Ray WA, Griffin MR, Fought RL et al (1992) Identification of fractures from computerized Medicare files. J Clin Epidemiol 45(7):703–714
Cummings SR, Black DM, Nevitt MC et al (1990) Appendicular bone density and age predict hip fracture in women. The Study of Osteoporotic Fractures Research Group. Jama 263(5):665–668
Kushi LH, Kaye SA, Folsom AR et al (1988) Accuracy and reliability of self-measurement of body girths. Am J Epidemiol 128(4):740–748
Potosky AL, Riley GF, Lubitz JD et al (1993) Potential for cancer related health services research using a linked Medicare-tumor registry database. Med Care 31(8):732–748
Magaziner J, Bassett SS, Hebel JR (1987) Predicting performance on the Mini-Mental State Examination. Use of age- and education-specific equations. J Am Geriatr Soc 35(11):996–1000
Teng EL, Chui HC (1987) The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry 48(8):314–318
Taylor BC, Schreiner PJ, Stone KL et al (2004) Long-term prediction of incident hip fracture risk in elderly white women: study of osteoporotic fractures. J Am Geriatr Soc 52(9):1479–1486
Schousboe JT, Fink HA, Taylor BC et al (2005) Association between self-reported prior wrist fractures and risk of subsequent hip and radiographic vertebral fractures in older women: a prospective study. J Bone Miner Res 20(1):100–106
Cummings SR, Nevitt MC, Browner WS et al (1995) Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med 332(12):767–773
Source of funding
The Study of Osteoporotic Fractures (SOF) is supported by the National Institutes of Health funding. The National Institute on Aging (NIA) provides support under the following grant numbers: R01 AG005407, R01 AR35582, R01 AR35583, R01 AR35584, R01 AG005394, R01 AG027574, and R01 AG027576. Dr. Curtis receives support from the NIH (AR053351) and the Agency for Healthcare Research and Quality (R01HS018517). The purchase of the linked CMS administrative claims data was supported, in part, by a grant to Dr. Curtis from the Arthritis Foundation.
Disclaimer
The views expressed herein do not necessarily represent the views of the Department of Veterans Affairs or the United States Government.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schousboe, J.T., Paudel, M.L., Taylor, B.C. et al. Magnitude and consequences of misclassification of incident hip fractures in large cohort studies: the Study of Osteoporotic Fractures and Medicare claims data. Osteoporos Int 24, 801–810 (2013). https://doi.org/10.1007/s00198-012-2210-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-012-2210-8