Abstract
The use of bone mineral density (BMD) for fracture discrimination may be improved by considering bone microarchitecture. Texture parameters such as trabecular bone score (TBS) or mean Hurst parameter (H) could help to find women who are at high risk of fracture in the non-osteoporotic group. The purpose of this study was to combine BMD and microarchitectural texture parameters (spine TBS and calcaneus H) for the detection of osteoporotic fractures. Two hundred and fifty five women had a lumbar spine (LS), total hip (TH), and femoral neck (FN) DXA. Additionally, texture analyses were performed with TBS on spine DXA and with H on calcaneus radiographs. Seventy-nine women had prevalent fragility fractures. The association with fracture was evaluated by multivariate logistic regressions. The diagnostic value of each parameter alone and together was evaluated by odds ratios (OR). The area under curve (AUC) of the receiver operating characteristics (ROC) were assessed in models including BMD, H, and TBS. Women were also classified above and under the lowest tertile of H or TBS according to their BMD status. Women with prevalent fracture were older and had lower TBS, H, LS-BMD, and TH-BMD than women without fracture. Age-adjusted ORs were 1.66, 1.70, and 1.93 for LS, FN, and TH-BMD, respectively. Both TBS and H remained significantly associated with fracture after adjustment for age and TH-BMD: OR 2.07 [1.43; 3.05] and 1.47 [1.04; 2.11], respectively. The addition of texture parameters in the multivariate models didn’t show a significant improvement of the ROC-AUC. However, women with normal or osteopenic BMD in the lowest range of TBS or H had significantly more fractures than women above the TBS or the H threshold. We have shown the potential interest of texture parameters such as TBS and H in addition to BMD to discriminate patients with or without osteoporotic fractures. However, their clinical added values should be evaluated relative to other risk factors.
Similar content being viewed by others
Introduction
In elderly populations, the incidence of osteoporotic fractures such as hip fracture shows a wide variation worldwide with an opposing trend East versus West [1]. Nevertheless, osteoporosis remains a major health concern with a significant impact on morbidity and quality of life [2]. Measurement of bone mineral density (BMD) is considered as the main approach for diagnosing osteoporosis and predicting fracture risk [3]. BMD is conventionally assessed with dual-energy X-ray absorptiometry (DXA). Currently, the World Health Organization (WHO) defines osteoporosis as a BMD T-score of −2.5 or less. However, according to this classification more than 50 % of incident fractures occur in osteopenic women (T-score between −1.0 and −2.5) or in women with normal BMD (T-score > −1.0) [4, 5]. Hence, bone density alone is not a sufficient fracture predictor. Osteoporotic fractures are related to the chance of having a low-energy fall [5]. Moreover, beyond bone mass, bone quality also contributes to bone strength. Consequently, osteoporosis has been redefined as a skeletal disorder characterized by a loss of bone density and bone quality associated with an increased risk of fracture [6, 7].
Bone quality is determined by a variety of mechanisms and its definition is still an open question. Among bone quality factors, bone microarchitecture has been identified to be of potential importance to explain fragility fractures. It was shown that among women who where matched for age and bone mineral content, women with vertebral fractures could be discriminated by three-dimensional microarchitecture parameters [8]. Although bone histomorphometry remains the gold standard to assess bone remodeling, its invasive nature does not allow its extensive use as a screening test to detect microarchitectural alterations. Micro-computed tomography, an ex vivo technique capable of a resolution of 6–10 µm voxel size, is often considered as the reference device to evaluate bone microarchitecture [9]. With advances in high-resolution techniques, some in vivo assessments of trabecular and cortical bone microarchitecture are possible [10]. Volumetric BMD assessed by high-resolution peripheral quantitative computed tomography (QCT) showed a good correlation with the areal BMD of DXA and could provide additional information about bone quality [11]. However, these techniques are limited to peripheral areas, excluding vertebrae and hip evaluation. In addition, current in vivo assessment of bone microarchitecture is limited by a linear voxel size of only 80–85 µm, which is too coarse to resolve individual trabeculae, even in peripheral sites. Because of its ability to assess cortical bone, QCT of the spine can also provide some improvement over spine BMD [12]. However, these devices are expensive, time-consuming, not always available in clinical practice, and have constraints of radiation dose. These are the limitations for their widespread use as complementary tests to improve the sensitivity of DXA in the detection of women who are at the risk of fracture. Accordingly, there is a need for more simple and convenient methods based on two-dimensional X-ray images, such as plain radiographs or bone scans produced by DXA. There is thus a growing interest in developing new gray-level features to detect changes in bone microarchitecture on two-dimensional images from osteoporotic fracture sites such as the spine and hip.
Fractal texture parameters assessed on high-resolution radiographs showed their ability to reflect microarchitecture and biomechanical bone properties [13–16]. New texture analyses named trabecular bone score (TBS) and mean Hurst parameter (H) have demonstrated a similar ability on low-resolution DXA devices [17–19] and on high-resolution devices [20], respectively. Independently, the TBS and the H parameter have been applied to improve fracture detection [21–24]. TBS is derived from the experimental variogram and evaluates the mean rate of gray-level variation considering a distance and a direction [25]. H is an oriented calculation of the Hurst exponent assuming a fractional Brownian field modeling of the image [26]. Both perform texture analysis on 2D projected images and both have demonstrated their relationship with 3D bone structures [20, 27]. TBS is assessed directly on the same DXA exams and on the same bone region used for the BMD assessment, whereas H is performed on calcaneus radiographs. The complementarity and clinical added values of H and TBS with BMD have been shown in cross-sectional [18, 23, 28, 29] and longitudinal studies [21, 22, 30, 31]. The aim of the present study was twofold. Firstly, we wanted to discriminate patients with osteoporotic fractures from those without fractures by means of texture parameters alone or in combination with BMD. Secondly, we were looking for improvement of the classification of postmenopausal women with and without fracture by means of a combination including TBS, H, and BMD.
Materials and Methods
Subjects
We conducted a retrospective, monocentric case–control study at the Hospital Center of Orleans (France). The study was conducted on 255 Caucasian postmenopausal women with mean age of 65 ± 12 years and an age range of 40–92 years. These patients were recruited from a French clinical research hospital program from November 2004 to February 2006. Patients were enrolled among the women attending the bone densitometry unit and the patients hospitalized in the rheumatology, orthopedic, and geriatric units. Subjects with wrist and hip fractures were recruited from the orthopedic surgery unit. The vertebral fracture cases came from the rheumatology and bone densitometry units. All patients (cases and controls) filled out an osteoporosis risk questionnaire (age, personal, and family history of fracture, tobacco and alcohol use, menopausal status, use of hormonal replacement therapy (HRT), treatment by oral corticosteroids, other medication, rheumatoid arthritis). Patients who were treated with corticosteroids, fluoride, bisphosphonates, HRT, tibolone, calcitonin, SERM, and PTH for more than 6 months in the previous year before inclusion were excluded. We also excluded patients with known diseases, which could interfere with bone metabolism: osteomalacia, bone cancer, myeloma, Paget’s disease, hyper parathyroidism, hyperthyroidism not treated, severe renal or hepatic insufficiency, prolonged immobilization (more than 2 months in the previous year before inclusion). The weight and height were measured and recorded at the visit of the DXA scan. Patients had a lumbar spine DXA scan and calcaneus radiograph. The women had a body mass index (BMI) between 15 and 41 kg/m2. Fragility fractures (spontaneous fractures or fractures after falls from standing height or less) were diagnosed according to radiologic data. The presence of vertebral fractures was diagnosed, using lateral spine radiographs according to Genant’s classification with grade II or more. Fractures which occurred before the age of 40 years and those of the face, fingers, toes, skull, and cervical spine were excluded. The fracture group was composed of all osteoporotic fractures including forearm, hip, humerus, shoulder, vertebral, and rib fractures. Among the 79 fractures there were 27 wrist fractures, 21 spine fractures, 13 femoral neck fractures, and 18 other osteoporotic fractures.
Bone Mineral Density Measurements
BMD was evaluated from lumbar spine (LS-BMD), femoral neck (FN-BMD), and total hip (TH-BMD) by DXA on Delphi (for 96 % of the scans), Discovery, and QDR 4500 devices (Hologic, Waltham, MA, USA). LS-BMD is the mean of individual measurements for vertebrae L1–L4 except for severe arthrosed or fractured vertebrae identified by a clinician who was experienced in DXA scan acquisition. TH-BMD and FN-BMD were assessed on the left hip and on the contralateral (non-fractured) femur in cases of hip fracture. Results were expressed in g/cm2 and T-score was calculated as the number of standard deviations above or below the mean BMD for young women.
Trabecular Bone Score analysis
All the raw images from the densitometer were sent to the University of Lausanne (Switzerland) for the calculation of Spine TBS blinded from clinical outcomes. TBS was calculated with the TBS iNsight Software v2.0 (Med-Imaps, Bordeaux, France) on the same vertebral region of interest (ROI) defined for the BMD measurement. TBS was obtained as the mean value of individual assessments for vertebrae L1, L2, L3, and L4. Fractured vertebrae were retrospectively excluded from the analysis. TBS was determined from the slope at the origin of the log–log plot of the experimental variogram. The variogram is the mean variation between two pixel intensity values with a separation vector, so includes both distance and direction [18].
Calcaneus Radiographs
High-resolution calcaneus digital radiographs were captured while the patient was placing the lateral part of the left heel in contact with the sensor of a direct digital X-ray device (BMA, D3A Medical Systems, Orleans, France). The acquisitions were obtained with the following standard characteristics: focal distance, 1.15 m and X-ray parameters, 55 kV and 20 mAs. The digital detector of the device had a 50 μm pixel size, leading to a spatial resolution of 8 line pairs per millimeter at 10 % modulation transfer function [32]. For each subject, the operator defined two anatomical landmarks: one at the upper point of the Achilles tendon insertion, and the second at the plantar aponevrosis insertion. These landmarks were used to create an ROI of 256 × 256 pixels (1.6 × 1.6 cm) located in the trabecular bone [33].
H Analysis
H was assessed by the digital X-ray device with the D3A Software on each calcaneus ROI. This software performed an oriented fractal analysis following 8 directions. For each of these directions, parallel lines were analyzed. The gray-level variations of these lines were modeled with a fractal model: the fractional Brownian motion [34]. The Hurst exponent of this model was estimated by the maximum likelihood estimator [35]. The H parameter for an image was measured as the mean value of the 8 angular direction estimations. Finally, a scattering correction was applied to this value.
Statistical Analysis
Means and 95 % confidence intervals (CI) were estimated for each of the two subject groups, women with fractures and women without fractures. Group differences were assessed by means of the nonparametric Wilcoxon signed-ranks test. A p value of 0.05 was set as the threshold for statistical significance. The relationships between BMD parameters, H, TBS, and biometric data were studied using the Spearman correlation. The diagnostic value of each parameter was further evaluated by multivariate logistic regression. Odds ratios (OR) expressed for each decrease of one standard deviation (SD) adjusted for age and additionally for TH-BMD, height, and weight were calculated. The area under curve (AUC) of the receiver operating characteristics (ROC) was used to evaluate the discrimination power of BMD, H, and TBS. For these estimates, OR 95 % CI and AUC 95 % CI were calculated. In addition, the minimum percentile of H and TBS (Min_TBS_H) was calculated. An evaluation associating both BMD and fractal parameters was conducted based on a logistic regression model including BMD with either TBS or H or Min_TBS_H. A first classification was carried out with BMD T-score stratification (minimum of spine or hip T-score) with three zones corresponding to thresholds defined by the WHO (i.e., T-score of −1.0 and −2.5 SDs). Furthermore, women in normal, osteopenic, osteoporotic, and non-osteoporotic groups were classified above and under the lowest tertile of H or TBS. The fracture prevalence was calculated by dividing the number of women with fractures by the number of women in each BMD category. According to the BMD status, the number of prevalent fractures below and above the first tertile was compared by χ 2 test.
Results
Description of Samples
Among the 255 postmenopausal women finally assessed, there were 79 women with prevalent fragility fractures. Women with prevalent fracture were older and shorter. Moreover, TBS, H, LS-BMD, and TH-BMD were lower in the group with fracture than in the group without fracture. No significant difference was found in BMI and weight (Table 1). Based on the WHO classification for the lowest of their BMD measurements at the LS or TH, our sample was composed of 102 women with normal BMD (40.0 %, aged 60.5 ± 10.5 years), 105 osteopenic women (41.2 %, aged 65.4 ± 11.0 years), and 48 osteoporotic women (18.8 %, aged 74.8 ± 9.9 years). In our study, 16.5 % of the women with prevalent fractures were in the normal range of BMD (fracture rate = 12.7 %), 43.0 % in the osteopenic range (fracture rate = 32.4 %), and 40.5 % were in the osteoporotic range (fracture rate = 66.7 %).
Correlation Between Clinical Parameters and Texture Parameters
TBS and H were positively correlated (r = 0.31, p < 0.0001). Positive correlations (Table 2) were obtained between LS-BMD with both H and TBS (p < 0.05 and p < 0.001, respectively). Correlations were also observed with FN-BMD and TH-BMD with both TBS and H (r value ranges from 0.41 to 0.48, p < 0.001). A positive correlation was obtained with both H and TBS with height (p < 0.0001). No significant correlations were obtained between TBS and weight and between H and BMI. Finally, negative correlations were obtained with FN-BMD, TH-BMD, TBS, and H with age (p < 0.001).
To a lesser extent, BMD and fractal parameters remained correlated with adjustments for age, height, and weight (Table 3). The partial correlation between H and TBS by controlling the influence of age, height, and weight remained significant (r = 0.19, p < 0.05).
Comparison of TBS or H Plus BMD
Odds ratios (OR) were estimated for TBS, H, and BMD with logistic regression model including age (Table 4). For LS-BMD, each incremental decrease of 1 SD was associated with more than 65 % increase of fracture risk in the OR for fracture status. For FN-BMD and TH-BMD, OR were 1.70 and 1.93, respectively. TBS and H were also significantly associated with fracture, with an OR of 2.25 and 1.72, respectively. Furthermore, both TBS and H remained significantly associated with fracture after additional adjustment for TH-BMD: OR 2.07 and 1.47, respectively. TH-BMD was included in the model since it had the best OR among the BMD parameters. Nevertheless, TBS and H also remained significantly associated with fracture after additional adjustments for LS-BMD: OR 2.02 [1.38; 3.04] and OR 1.57 [1.12; 2.22], respectively. The combination of TBS and H was also significantly associated with fracture after additional adjustments for TH-BMD and each of these texture parameters (i.e., H for TBS and TBS for H), with an OR of 2.06 and 1.46, respectively and after additional adjustments for TH-BMD, weight, height, and each of these texture parameters with OR 1.83 and 1.48, respectively.
In multivariate logistic regression models including age, weight, and height (Fig. 1), the AUCs were 79.5, 78.3, 79.9, and 80.6 % for TH-BMD, H, TBS, and Min_TBS_H, respectively. With additional inclusion of TH-BMD, AUCs were 81.0, 81.4, 81.8 % for H, TBS, and Min_TBS_H, respectively. Significant differences between the TH-BMD model and the H, TBS, and Min_TBS_H models were borderline (p = 0.09, p = 0.12, and p = 0.06, respectively).
ROC curve in the whole population. All multivariate models included age, weight, and height. All AUCs (CI 95 %) differ from 50 % significantly (p < 0.001). a TH-BMD. b H + TH-BMD model, c TBS + TH-BMD model, and d Min_TBS_H + TH-BMD. TH-BMD total hip bone mineral density, TBS trabecular bone score, H mean Hurst parameter, Min_TBS_H minimum of TBS and H
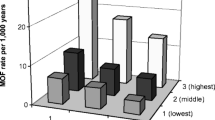
Regarding H, 54 % of fractures occurred in the lowest tertile (<0.615), with a fracture rate of 51.1 %. Compared with women whose H was above the lowest tertile limit, the prevalence was significantly greater (51.1 vs. 20.4 %, p < 0.001, Fig. 2). Moreover, the prevalence of fracture in osteopenic women with a H in the lowest tertile compared with osteopenic women with their H in the highest tertiles was significantly different (45.5 vs. 23.0 %, p = 0.03). Twenty-four women with fractures out of 43 who were in the lowest range of H, were considered as healthy (n = 4) or osteopenic (n = 20) by BMD (fracture prevalence = 41.4 %, corresponding to 30.4 % of the fractures observed in our study).
Regarding TBS, 56 % of fractures occurred in the lowest tertile (<1.186), with a fracture rate of 51.8 %. Compared with women whose TBS was above the lowest tertile limit, the prevalence was significantly greater (51.8 vs. 20.6 %, p < 0.001, Fig. 3). Moreover, the prevalence of fracture in osteopenic women with a TBS in the lowest tertile compared with osteopenic women with their TBS in the highest tertiles was not significantly different (42.1 vs. 26.9 %, p = 0.17). Twenty women with fractures out of 44 who were in the lowest range of TBS were considered as healthy (n = 4) or osteopenic (n = 16) by BMD (fracture prevalence = 38.5 %, corresponding to 25.3 % of the fractures observed in our study).
Women with normal or osteopenic BMD in the lowest range of TBS or H had significantly more fractures than women above the TBS or the H threshold (17.4 vs. 38.5 %, p = 0.003 and 15.4 vs. 41.4 %, p = 0.0001, respectively, Figs. 2 and 3). Similarly, in the non-osteoporotic group, women in the lowest range of Min_TBS_H had significantly more fractures than women in the highest tertiles of Min_TBS_H (44.0 vs.16.0 %, p = 0.00008).
Discussion
Both TBS and H remained significantly associated with fractures after inclusion of TH-BMD. The ROC-AUC differences were significantly borderline between multivariate models with TH-BMD and multivariate models with TH-BMD and H or TBS (p = 0.09, p = 0.12, respectively). The combination of BMD and texture parameters led to a weak global improvement. However, AUC differences are very small in magnitude when powerful risk factors are already in the model such as age and TH-BMD. In addition, in the non-osteoporotic group, the number of fractures was significantly greater below than above the lowest tertile of TBS or H. Thus, the texture parameters could help to classify a subset of non-osteoporotic women into a group with a higher risk of fractures but their usefulness should be compared with other risk factors.
Several clinical studies have already shown the ability of TBS or H separately to discriminate patients with fragility fractures from those without fractures. In the very large Canadian study in which 29,407 women from the province of Manitoba were enrolled [22], both spine TBS and LS-BMD predicted osteoporotic fractures (OR 1.45 and OR 1.72, respectively). It was also demonstrated that spine TBS provides information independent of spine BMD and clinical risk factors and that their combination improves the fracture prediction in this population [22]. In a Japanese postmenopausal women cohort, it was found that spine TBS was lower in women with vertebral fracture relative to women without fracture and OR remained significant after adjusting for both lumbar spine areal BMD and other clinical risk factors [30].
In a case–control study, it has been shown that fractal analysis on calcaneus radiographs was able to discriminate osteoporotic women with vertebral fractures from controls including in subgroups with overlapping FN-BMD or trochanteric BMD values [36]. Furthermore, a multi-centric cross-sectional study reported that H values were significantly lower in osteoporotic fracture cases than in control cases. Such differences persisted after adjustment for TH-BMD. In addition, using ROC-AUC no significant differences were found between TH-BMD and H [23].
LS-BMD and TBS were positively correlated (r = 0.52). This correlation was higher than in the Canadian study (DXA with Lunar device) (r = 0.32). This variability has already been highlighted [21] with potential differences between Hologic and GE-Lunar devices. In our study, 96 % of the DXA scans came from the same device (Delphi Hologic) and all the DXA were done on a device from the same manufacturer. Our TBS values were comparable with those reported in other studies [21, 22]. Moreover, the correlation between H and FN-BMD (r = 0.41) was comparable with the one found in a previous study [14] (r = 0.44). We used TBS thresholds coming from the tertile classification (1.186 and 1.300) near actual cutoff points used in many studies [19]. For all texture parameters (H, TBS, and Min_TBS_H), we used the tertile thresholds in order to allow comparisons.
The main clinical interest of texture analysis is to better identify women at risk of fracture in particular those having a BMD above the traditional clinical threshold of −2.5 T-score. In the Manitoba cohort [22], the population was stratified using tertiles of lumbar spine TBS and the WHO classification for LS-BMD. The authors showed that being in the minimum tertile was a significant predictor of fractures. In our study, we followed this scheme by dividing TBS, H, and Min_TBS_H in tertiles. Thus, the texture parameters TBS, H, and Min_TBS_H in combination with BMD showed an ability to classify patients with fractures among the non-osteoporotic women group.
In addition, we studied the combination of both H and TBS with the BMD. On the one hand, both TBS and H remained significantly associated with fracture after additional adjustments for TH-BMD, weight, height, and each of these texture parameters (i.e., H with TBS and vice versa), with OR of 1.83 and 1.48, respectively. On the other hand, the two texture parameters were correlated with r = 0.31 (p < 0.0001), explaining less than 10 % of its variance. These results could be explained either by the fact that the two parameters were assessed at different bone sites (accounting for different types of trabecular bone) or by the fact that these parameters measured different bone properties.
Our study has showed some limitations. Our sample of patients with fractures was rather low and may explain the borderline significance of improvement in AUC when we added fractal parameters. Other risk factors should be studied such as physical activity, muscle function, past falls, and parental history of fracture [37]. The comparison with FRAX could be interesting to evaluate the performance of this combination of texture parameters among the other risk factors. Unfortunately, given the small number of fractures in each usual site of osteoporotic fracture (i.e., 27 wrists, 21 spines, 13 femoral necks, and 18 others), this study was based on a group of women with different types of fractures. It is unclear how our analysis may apply to the clinical situation of an individual woman and her risk of having a vertebral or hip fracture. Furthermore, in this protocol, images were acquired by two different medical imaging modalities. So, it is difficult to know if the independence between H and TBS values was associated with different aspects of microarchitecture. In addition, H requires a new measurement of the heel with additional time, expense, and radiation exposure (2.7 μSv). OR values showed that TBS was more associated with fracture than H but the latter parameter was not assessed on a site of osteoporotic fractures. As explained above, TBS and H were evaluated with different algorithms. Thus, it would be interesting to combine the assessment of H and TBS for the same bone site and with the same bone imaging device to allow direct comparison.
Despite these limitations, this study showed the potential interest of texture parameters such as TBS and H in addition to BMD to discriminate patients with osteoporotic fractures from those without fractures. The texture features of bone could help to find women at high risk of fracture in the non-osteoporotic group.
References
Ballane G, Cauley JA, Luckey MM, Fuleihan GE-H (2014) Secular trends in hip fractures worldwide: opposing trends East versus West. J Bone Miner Res 29(8):1745–1755
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17(12):1726–1733
Marshall D, Johnell O, Wedel H (1996) Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 312(7041):1254–1259
Schuit SC, van der Klift M, Weel AEA, de Laet CED, Burger H, Seeman E et al (2004) Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam study. Bone 34(1):195–202
Sornay-Rendu E, Munoz F, Garnero P, Duboeuf F, Delmas PD (2005) Identification of osteopenic women at high risk of fracture: the OFELY study. J Bone Miner Res 20(10):1813–1819
Ott SM, Kilcoyne RF, Chesnut CH (2009) Ability of four different techniques of measuring bone mass to diagnose vertebral fractures in postmenopausal women. J Bone Miner Res 2(3):201–210
NIH Consensus Development Panel on Osteoporosis Prevention (2001) Diagnosis, and therapy. Osteoporosis prevention, diagnosis, and therapy. J Am Med Assoc 285(6):785–795
Kleerekoper M, Villanueva AR, Stanciu J, Rao DS, Parfitt AM (1985) The role of three-dimensional trabecular microstructure in the pathogenesis of vertebral compression fractures. Calcif Tissue Int 37(6):594–597
Bouxsein ML, Boyd SK, Christiansen BA, Guldberg RE, Jepsen KJ, Müller R (2010) Guidelines for assessment of bone microstructure in rodents using micro-computed tomography. J Bone Miner Res 25(7):1468–1486
Boutroy S, Bouxsein ML, Munoz F, Delmas PD (2005) In vivo assessment of trabecular bone microarchitecture by high-resolution peripheral quantitative computed tomography. J Clin Endocrinol Metab 90(12):6508–6515
MacNeil JA, Boyd SK (2007) Accuracy of high-resolution peripheral quantitative computed tomography for measurement of bone quality. Med Eng Phys 29(10):1096–1105
Melton LJ, Riggs BL, Keaveny TM, Achenbach SJ, Hoffmann PF, Camp JJ et al (2007) Structural determinants of vertebral fracture risk. J Bone Miner Res 22(12):1885–1892
Lespessailles E, Roux JP, Benhamou CL, Arlot ME, Eynard E, Harba R et al (1998) Fractal analysis of bone texture on os calcis radiographs compared with trabecular microarchitecture analyzed by histomorphometry. Calcif Tissue Int 63:121–125
Le Corroller T, Halgrin J, Pithioux M, Guenoun D, Chabrand P, Champsaur P (2011) Combination of texture analysis and bone mineral density improves the prediction of fracture load in human femurs. Osteoporos Int 23(1):163–169
Kolta S, Paratte S, Amphoux T, Persohn S, Campana S, Skalli W et al (2011) Bone texture analysis of human femurs using a new device (BMA™) improves failure load prediction. Osteoporos Int 23(4):1311–1316
Guenoun D, Le Corroller T, Acid S, Pithioux M, Pauly V, Ariey-Bonnet D et al (2013) Radiographical texture analysis improves the prediction of vertebral fracture: an ex vivo biomechanical study. Spine 38(21):E1320–E1326
Roux JP, Wegrzyn J, Boutroy S, Bouxsein ML, Hans D, Chapurlat R (2013) The predictive value of trabecular bone score (TBS) on whole lumbar vertebrae mechanics: an ex vivo study. Osteoporos Int 24(9):2455–2460
Winzenrieth R, Dufour R, Pothuaud L, Hans D (2009) A retrospective case-control study assessing the role of trabecular bone score in postmenopausal caucasian women with osteopenia: analyzing the odds of vertebral fracture. Calcif Tissue Int 86(2):104–109
Silva BC, Leslie WD, Resch H, Lamy O, Lesnyak O, Binkley N et al (2014) trabecular bone score: a noninvasive analytical method based upon the dxa image. J Bone Miner Res 29(3):518–530
Jennane R, Harba R, Lemineur G, Bretteil S, Estrade A, Benhamou CL (2007) Estimation of the 3D self-similarity parameter of trabecular bone from its 2D projection. Med Image Anal 11(1):91–98
Boutroy S, Hans D, Sornay-Rendu E, Vilayphiou N, Winzenrieth R, Chapurlat R (2012) Trabecular bone score improves fracture risk prediction in non-osteoporotic women: the OFELY study. Osteoporos Int 24(1):77–85
Hans D, Goertzen AL, Krieg M-A, Leslie WD (2011) Bone microarchitecture assessed by TBS predicts osteoporotic fractures independent of bone density: the manitoba study. J Bone Miner Res 26(11):2762–2769
Lespessailles E, Gadois C, Kousignian I, Neveu JP, Fardellone P, Kolta S et al (2008) Clinical interest of bone texture analysis in osteoporosis: a case control multicenter study. Osteoporos Int 19(7):1019–1028
Benhamou C-L, Poupon S, Lespessailles E, Loiseau S, Jennane R, Siroux V et al (2001) Fractal analysis of radiographic trabecular bone texture and bone mineral density: two complementary parameters related to osteoporotic fractures. J Bone Miner Res 16(4):697–704
Bousson V, Bergot C, Sutter B, Levitz P, Cortet B, Scientific Committee of the Groupe de Recherche et d’Information sur les Ostéoporoses (2012) Trabecular bone score (TBS): available knowledge, clinical relevance, and future prospects. Osteoporos Int. 23(5):1489–1501
Jennane R, Ohley WJ, Majumdar S, Lemineur G (2001) Fractal analysis of bone X-ray tomographic microscopy projections. IEEE Trans Med Imaging 20(5):443–449
Pothuaud L, Carceller P, Hans D (2008) Correlations between grey-level variations in 2D projection images (TBS) and 3D microarchitecture: applications in the study of human trabecular bone microarchitecture. Bone 42(4):775–787
Rabier B, Héraud A, Grand-Lenoir C, Winzenrieth R, Hans D (2010) A multicentre, retrospective case–control study assessing the role of trabecular bone score (TBS) in menopausal Caucasian women with low areal bone mineral density (BMDa): analysing the odds of vertebral fracture. Bone 46(1):176–181
Pothuaud L, Barthe N, Krieg M-A, Mehsen N, Carceller P, Hans D (2009) Evaluation of the potential use of trabecular bone score to complement bone mineral density in the diagnosis of osteoporosis: a preliminary spine bmd–matched, case-control study. J Clin Densitom 12(2):170–176
Iki M, Tamaki J, Kadowaki E, Sato Y, Dongmei N, Winzenrieth R et al (2014) Trabecular bone score (TBS) predicts vertebral fractures in Japanese women over 10 years independently of bone density and prevalent vertebral deformity: the Japanese population-based osteoporosis (JPOS) cohort study. J Bone Miner Res 29(2):399–407
Briot K, Paternotte S, Kolta S, Eastell R, Reid DM, Felsenberg D et al (2013) Added value of trabecular bone score to bone mineral density for prediction of osteoporotic fractures in postmenopausal women: the OPUS study. Bone 57(1):232–236
Lespessailles E, Gadois C, Lemineur G, Do-Huu JP, Benhamou L (2007) Bone texture analysis on direct digital radiographic images: precision study and relationship with bone mineral density at the os calcis. Calcif Tissue Int 80(2):97–102
Benhamou CL, Lespessailles E, Jacquet G, Harba R, Jennane R, Loussot T et al (1994) Fractal organization of trabecular bone images on calcaneus radiographs. J Bone Miner Res 9(12):1909–1918
Mandelbrot BB, Van Ness JW (1968) Fractional brownian motions, fractional noises and applications. SIAM Rev 10(4):422–437
Lundahl T, Ohley WJ, Kay SM, Siffert R (1986) Fractional brownian motion: a maximum likelihood estimator and its application to image texture. IEEE Trans Med Imaging 5(3):152–161
Pothuaud L, Lespessailles E, Harba R, Jennane R, Royant V, Eynard E et al (1998) Fractal analysis of trabecular bone texture on radiographs: discriminant value in postmenopausal osteoporosis. Osteoporos Int 8:618–625
Albrand G, Munoz F, Sornay-Rendu E, DuBoeuf F, Delmas PD (2003) Independent predictors of all osteoporosis-related fractures in healthy postmenopausal women: the OFELY study. Bone 32(1):78–85
Acknowledgments
We are grateful to Farida Khacef and Nathalie Villequenault for their help in this study.
Conflict of interest
R. Winzenrieth is employed by the Med-Imaps group. J. Chaintreuil was employed at D3A Medical Systems when the work was initiated, then at the Med-Imaps group. D. Hans is CEO of the Med-Imaps group, co-owner of the TBS patent, and has corresponding ownership shares in the Med-Imaps group. J. Touvier, H. Johansson, H. Toumi, J. P. Roux, R. Jennane, and E. Lespessailles have declared no conflicts of interest.
Human and Animal Rights and Informed Consent
This study is in accordance with the Declaration of Helsinki and the International Conference on Harmonization of Good Clinical Practice Guidelines. Additionally, the protocol was approved by an independent regional ethics committee. All the patients and control women entered into the study after written informed consent.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Touvier, J., Winzenrieth, R., Johansson, H. et al. Fracture Discrimination by Combined Bone Mineral Density (BMD) and Microarchitectural Texture Analysis. Calcif Tissue Int 96, 274–283 (2015). https://doi.org/10.1007/s00223-015-9952-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-015-9952-1