Abstract
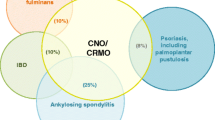
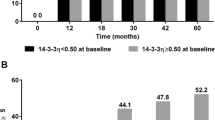
Chronic recurrent multifocal osteomyelitis (CRMO), the most severe form of chronic nonbacterial osteomyelitis, is an autoinflammatory bone disorder. A timely diagnosis and treatment initiation is complicated by the absence of widely accepted diagnostic criteria and an incomplete pathophysiological understanding. The aim of this study was to determine biomarkers for the diagnosis and follow-up of CRMO. Serum of 56 CRMO patients was collected at the time of diagnosis. As controls, sera from treatment-naïve age-matched patients with Crohn’s disease (N = 62) or JIA (N = 28) as well as healthy individuals (N = 62) were collected. Multiplex analysis of 25 inflammation markers was performed. Statistical analysis was performed using Kruskal–Wallis and Mann–Whitney U tests, canonical discriminant analysis, and mixed model variance analysis. Mostly monocyte-derived serum proteins were detectable and differed significantly between groups: IL-1RA, IL-2R, IL-6, IL-12, eotaxin, MCP-1, MIP-1b, RANTES. Multicomponent discriminant analysis allowed for the definition of algorithms differentiating between CRMO, Crohn’s disease, and healthy controls. Persistently high levels of MCP-1, IL-12, sIL-2R correlated with incomplete remission in follow-up samples from CRMO patients. Discrimination algorithms allow differentiation between patients with CRMO or Crohn’s disease, and healthy individuals. IL-12, MCP-1, and sIL-2R can act as markers for treatment response. Though confirmation of our findings in larger multiethnical cohorts is warranted, they may prove valuable to differentiate between otherwise healthy individuals or Crohn’s disease patients with “bone pain” and CRMO patients. The elevation of mainly monocyte-derived pro-inflammatory serum proteins supports the hypothesis of pro-inflammatory monocyte/macrophages driving inflammation in CRMO.





Similar content being viewed by others
Abbreviations
- CNO:
-
Chronic nonbacterial osteomyelitis
- CRMO:
-
Chronic recurrent multifocal osteomyelitis
- CRP:
-
C-reactive protein
- Eotaxin:
-
C-C motif chemokine 11, also known as eosinophil chemotactic protein and eotaxin-1
- ESR:
-
Erythrocyte sedimentation rate
- GM-CSF:
-
Granulocyte macrophage colony stimulating factor
- IFN:
-
Interferon
- IL:
-
Interleukin
- IL-1RA:
-
IL-1 receptor antagonist
- JIA:
-
Juvenile idiopathic arthritis
- sIL-2R:
-
Soluble IL-2 receptor
- IP-10:
-
Interferon gamma-induced protein 10, also known as C-X-C motif chemokine 10 (CXCL10)
- MCP-1:
-
Monocyte chemotactic protein 1
- MIG:
-
Monokine induced by gamma-interferon, also known as Chemokine (C-X-C motif) ligand 9 (CXCL9)
- MIP:
-
Macrophage inflammatory protein
- RANTES:
-
Regulated on activation, normal T cell expressed and secreted protein, also known as Chemokine (C-C motif) ligand 5 (CCL5)
- TNF-α:
-
Tumor necrosis factor α
References
Hedrich CM, Hahn G, Girschick HJ, Morbach H (2013) A clinical and pathomechanistic profile of chronic nonbacterial osteomyelitis/chronic recurrent multifocal osteomyelitis and challenges facing the field. Expert Rev Clin Immunol 9(9):845–854
Hedrich CM, Hofmann SR, Pablik J, Morbach H, Girschick HJ (2013) Autoinflammatory bone disorders with special focus on chronic recurrent multifocal osteomyelitis (CRMO). Pediatr Rheumatol Online J 11(1):47
Stern SM, Ferguson PJ (2013) Autoinflammatory bone diseases. Rheum Dis Clin North Am 39(4):735–749
Chitu V, Ferguson PJ, de Bruijn R, Schlueter AJ, Ochoa LA, Waldschmidt TJ et al (2009) Primed innate immunity leads to autoinflammatory disease in PSTPIP2-deficient cmo mice. Blood 114(12):2497–2505
Ferguson PJ, Bing X, Vasef MA, Ochoa LA, Mahgoub A, Waldschmidt TJ et al (2006) A missense mutation in pstpip2 is associated with the murine autoinflammatory disorder chronic multifocal osteomyelitis. Bone 38(1):41–47
Chitu V, Nacu V, Charles JF, Henne WM, McMahon HT, Nandi S et al (2012) PSTPIP2 deficiency in mice causes osteopenia and increased differentiation of multipotent myeloid precursors into osteoclasts. Blood 120(15):3126–3135
Grosse J, Chitu V, Marquardt A, Hanke P, Schmittwolf C, Zeitlmann L et al (2006) Mutation of mouse Mayp/Pstpip2 causes a macrophage autoinflammatory disease. Blood 107(8):3350–3358
Hofmann SR, Roesen-Wolff A, Hahn G, Hedrich CM (2012) Update: cytokine dysregulation in chronic nonbacterial osteomyelitis (CNO). Int J Rheumatol 2012:310206
Hofmann SR, Morbach H, Schwarz T, Rosen-Wolff A, Girschick HJ, Hedrich CM (2012) Attenuated TLR4/MAPK signaling in monocytes from patients with CRMO results in impaired IL-10 expression. Clin Immunol 145(1):69–76
Hamel J, Paul D, Gahr M, Hedrich CM (2012) Pilot study: possible association of IL10 promoter polymorphisms with CRMO. Rheumatol Int 32(2):555–556
Hofmann SR, Schwarz T, Moller JC, Morbach H, Schnabel A, Rosen-Wolff A et al (2011) Chronic non-bacterial osteomyelitis is associated with impaired Sp1 signaling, reduced IL10 promoter phosphorylation, and reduced myeloid IL-10 expression. Clin Immunol 141(3):317–327
Jansson AF, Muller TH, Gliera L, Ankerst DP, Wintergerst U, Belohradsky BH et al (2009) Clinical score for nonbacterial osteitis in children and adults. Arthritis Rheum 60(4):1152–1159
Girschick HJ, Zimmer C, Klaus G, Darge K, Dick A, Morbach H (2007) Chronic recurrent multifocal osteomyelitis: what is it and how should it be treated? Nat Clin Pract Rheumatol 3(12):733–738
Beck C, Morbach H, Beer M, Stenzel M, Tappe D, Gattenlohner S et al (2010) Chronic nonbacterial osteomyelitis in childhood: prospective follow-up during the first year of anti-inflammatory treatment. Arthritis Res Ther 12(2):R74
McInnes IB (2013) Cytokines. In: Firestein GS Budd R, Harris Ed Jr (ed) Kelley´s textbook of rheumatology, 9th Edition. Elsevier Sanders, Philadelphia, pp 367–377
Eulenfeld R, Dittrich A, Khouri C, Muller PJ, Mutze B, Wolf A et al (2012) Interleukin-6 signalling: more than Jaks and STATs. Eur J Cell Biol 91(6–7):486–495
Hamza T, Barnett JB, Li B (2010) Interleukin 12 a key immunoregulatory cytokine in infection applications. Int J Mol Sci 11(3):789–806
Griffith JW, Sokol CL, Luster AD (2014) Chemokines and chemokine receptors: positioning cells for host defense and immunity. Annu Rev Immunol 32:659–702
Chen W, Paulus B, Shu D, Wilson I, Chadwick V (2001) Increased serum levels of eotaxin in patients with inflammatory bowel disease. Scand J Gastroenterol 36(5):515–520
Rehman MQ, Beal D, Liang Y, Noronha A, Winter H, Farraye FA et al (2013) B cells secrete eotaxin-1 in human inflammatory bowel disease. Inflamm Bowel Dis 19(5):922–933
Hofmann SR, Rosen-Wolff A, Tsokos GC, Hedrich CM (2012) Biological properties and regulation of IL-10 related cytokines and their contribution to autoimmune disease and tissue injury. Clin Immunol 143(2):116–127
Glocker EO, Kotlarz D, Klein C, Shah N, Grimbacher B (2011) IL-10 and IL-10 receptor defects in humans. Ann N Y Acad Sci 1246:102–107
Hedrich CM, Bream JH (2010) Cell type-specific regulation of IL-10 expression in inflammation and disease. Immunol Res 47(1–3):185–206
Bruck N, Schnabel A, Hedrich CM (2015) Current understanding of the pathophysiology of systemic juvenile idiopathic arthritis (sJIA) and target-directed therapeutic approaches. Clin Immunol 159(1):72–83
Niehues T, Feyen O, Telieps T (2008) Concepts on the pathogenesis of juvenile idiopathic arthritis. Z Rheumatol 67(2):111–116
Hofmann SR, Kubasch AS, Ioannidis C, Rosen-Wolff A, Girschick HJ, Morbach H et al (2015) Altered expression of IL-10 family cytokines in monocytes from CRMO patients result in enhanced IL-1beta expression and release. Clin Immunol 161(2):300–307
Barranco C (2014) Experimental arthritis: link between IL-10 and activation of the NLRP3 inflammasome in the synovium. Nat Rev Rheumatol 10(10):576
Greenhill CJ, Jones GW, Nowell MA, Newton Z, Harvey AK, Moideen AN et al (2014) Interleukin-10 regulates the inflammasome-driven augmentation of inflammatory arthritis and joint destruction. Arthritis Res Ther 16(4):419
Acknowledgments
The authors thank Prof. Dr. Ezio Bonifacio and Carmen Wilhelm for their support during Luminex® analysis and Christine Hedrich for valuable discussion and editing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Compliance with ethical standards
C. M. H. participated in an advisory board meeting by Novartis Pharmaceuticals on the pathophysiology and treatment of systemic JIA. The authors declare that they have no competing interests. The authors declare no relevant financial conflict of interest relevant to this manuscript. The study was supported by the MeDDrive 2014 program, Faculty of Medicine Carl Gustav Carus, TU Dresden (Grant Number: 60.343), and the Novartis Foundation for Therapeutic Research (both grants to C.M.H.). All individuals and/or their parents or legal guardians gave written informed consent. Sample collection and use were approved by the ethics committees of the University of Würzburg (CRMO, JIA patients, and controls) and the University of Technology Dresden/Technische Universität Dresden (Crohn’s disease).
Additional information
Sigrun Renate Hofmann and Anne Sophie Kubasch have contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hofmann, S.R., Kubasch, A.S., Range, U. et al. Serum biomarkers for the diagnosis and monitoring of chronic recurrent multifocal osteomyelitis (CRMO). Rheumatol Int 36, 769–779 (2016). https://doi.org/10.1007/s00296-016-3466-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-016-3466-7