Abstract
Background and Aims
Inflammatory bowel disease (IBD) is associated with impaired health-related quality of life (HRQOL) and adherence. Our aim was to identify demographic, clinical, and psychosocial predictors of impaired HRQOL and non-adherence to provider recommendations.
Methods
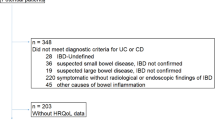
Adults with Crohn’s disease (CD) or ulcerative colitis (UC) residing within the USA were recruited from online IBD support groups for participation in this cross-sectional study. Data were collected online through standardized instruments, including the Inflammatory Bowel Disease Questionnaire and the Medical Outcomes Study (MOS) general adherence scale. Bivariate analyses and multivariate linear regression were used to assess predictors of HRQOL and adherence.
Results
We recruited 136 individuals, among whom median age was 35 years (range 18–75), and 82 % were female. 57 % had CD, and 43 % had UC. Predictors of lower HRQOL among CD patients were perceived stress (p < 0.0001), number of CD relapses (p < 0.0001), and female gender (p = 0.0015), while among UC patients they were perceived stress (p < 0.0001) and number of UC relapses (p = 0.0017). Predictors of lower adherence to provider recommendations in CD were perceived stress (p = 0.0007) and older age (p = 0.041), while in UC, perceived stress was the only predictor of lower adherence (p = 0.022).
Conclusions
Among patients with IBD, a higher level of perceived stress is a strong predictor of lower HRQOL and lower adherence to provider recommendations. Additionally, females with CD and patients with higher number of IBD relapses may be at risk of lower HRQOL. Psychological interventions, including physician-facilitated conversations, psychological screeners, and a multidisciplinary approach, may help address impaired HRQOL and adherence and merit further study.


Similar content being viewed by others
References
De Schepper HU, De Man JG, Moreels TG, Pelckmans PA, De Winter BY. Review article: gastrointestinal sensory and motor disturbances in inflammatory bowel disease—clinical relevance and pathophysiological mechanisms. Aliment Pharmacol Ther. 2008;27:621–637.
Baumgart DC, Sandborn WJ. Inflammatory bowel disease: clinical aspects and established and evolving therapies. Lancet. 2007;369:1641–1657.
Devlen J, Beusterien K, Yen L, Ahmed A, Cheifetz AS, Moss AC. The burden of inflammatory bowel disease: a patient-reported qualitative analysis and development of a conceptual model. Inflamm Bowel Dis. 2014;20:545–552.
Dudley-Brown S. Prevention of psychological distress in persons with inflammatory bowel disease. Issues Ment Health Nurs. 2002;23:403–422.
Sainsbury A, Heatley RV. Review article: psychosocial factors in the quality of life of patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2005;21:499–508.
Van der Have M, van der Aalst KS, Kaptein AA, et al. Determinants of health-related quality of life in Crohn’s disease: a systematic review and meta-analysis. J Crohns Colitis. 2014;8:93–106.
Casellas F, López-Vivancos J, Casado A, et al. Factors affecting health related quality of life of patients with inflammatory bowel disease. Qual Life Res. 2002;11:775–781.
Robinson A. Review article: improving adherence to medication in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2008;27:9–14.
Devlen J, Beusterien K, Yen L, Ahmed A, Cheifetz AS, Moss AC. Barriers to mesalamine adherence in patients with inflammatory bowel disease: a qualitative analysis. J Manag Care Pharm. 2014;20:309–314.
Van der Eijk I, Stockbrügger R, Russel M. Influence of quality of care on quality of life in inflammatory bowel disease (IBD): literature review and studies planned. Eur J Intern Med. 2000;11:228–234.
Irvine EJ. Quality of life issues in patients with inflammatory bowel disease. Am J Gastroenterol. 1997;92:18S–24S.
Drossman DA, Patrick DL, Mitchell CM, et al. Health-related quality of life in inflammatory bowel disease. Functional status and patient worries and concerns. Dig Dis Sci. 1989;34:1379–1386.
Moradkhani A, Beckman LJ, Tabibian JH. Health-related quality of life in inflammatory bowel disease: psychosocial, clinical, socioeconomic, and demographic predictors. J Crohns Colitis. 2013;7:467–473.
Jaghult S, Saboonchi F, Johansson U, Wredling R, Kapraali M. Identifying predictors of low health related quality of life among patients with inflammatory bowel disease: comparison between Crohn’s disease and ulcerative colitis with disease duration. J Clin Nurs. 2011;20:1578–1587.
Rubin G, Hungin AP, Chinn D, et al. Long-term aminosalicylate therapy is under-used in patients with ulcerative colitis: a cross-sectional survey. Aliment Pharmacol Ther. 2002;16:1889–1893.
Bernal I, Domènech E, Garcia-Planella E, et al. Medication-taking behaviour in a cohort of patients with inflammatory bowel disease. Dig Dis Sci. 2006;51:2165–2169.
San-Román AL, Bermejo F, Carrera E, Pérez-Abad M, Boixeda D. Adherence to treatment in inflammatory bowel disease. Rev Esp Enferm Dig. 2005;97:249–257.
Selinger CP, Eaden J, Jones DB, et al. Modifiable factors associated with nonadherence to maintenance medication for inflammatory bowel disease. Inflamm Bowel Dis. 2013;19:2199–2206.
Hawthorne AB, Rubin G, Ghosh S. Review article: medication non-adherence in ulcerative colitis—strategies to improve adherence with mesalazine and other maintenance therapies. Aliment Pharmacol Ther. 2008;27:1157–1166.
Shale MJ, Riley SA. Studies of compliance with delayed-release mesalazine therapy in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2003;18:191–198.
Thia K, Faubion WA, Loftus EV, Persson T, Persson A, Sandborn WJ. Short CDAI: development and validation of a shortened and simplified Crohn’s Disease Activity Index. Inflamm Bowel Dis. 2011;17:105–111.
Walmsley RS, Ayers RCS, Pounder RE, Allan RN. A simple clinical colitis activity index. Gut. 1998;43:29–32.
Higgins PDR, Schwartz M, Mapili J, Krokos I, Leung J, Zimmermann EM. Patient defined dichotomous end points for remission clinical improvement in ulcerative colitis. Gut. 2005;54:782–788.
Guyatt G, Mitchell A, Irvine JE, et al. A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterology. 1989;96:804–810.
Kravitz RL, Hays RD, Sherbourne CD, et al. Recall of recommendations and adherence to advice among patients with chronic medical conditions. Arch Intern Med. 1993;153:1869–1878.
Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, eds. The Social Psychology of Health. Newbury Park, CA: Sage; 1988.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:386–396.
Eaden JA, Abrams K, Mayberry JF. The Crohn’s and colitis knowledge score: a test for measuring patient knowledge in inflammatory bowel disease. Am J Gastroenterol. 1999;94:3560–3566.
Duffy LC, Zielezny MA, Marshall JR, et al. Lag time between stress events and risk of recurrent episodes of inflammatory bowel disease. Epidemiology. 1991;2:141–145.
Levenstein S, Prantera C, Varvo V, et al. Stress and exacerbation in ulcerative colitis: a prospective study of patients enrolled in remission. Am J Gastroenterol. 2000;95:1213–1220.
Bitton A, Sewitch MJ, Peppercorn MA, et al. Psychosocial determinants of relapse in ulcerative colitis: a longitudinal study. Am J Gastroenterol. 2003;98:2203–2208.
Bitton A, Dobkin P, Edwardes MD, et al. Predicting relapse in Crohn’s disease: a biopsychosocial model. Gut. 2008;57:1386–1392.
Graff LA, Walker JR, Clara I, et al. Stress coping, distress, and health perceptions in inflammatory bowel disease and community controls. Am J Gastroenterol. 2009;104:2959–2969.
Rogala L, Miller N, Graff LA, et al. Population-based controlled study of social support, self-perceived stress, activity and work issues, and access to health care in inflammatory bowel disease. Inflamm Bowel Dis. 2008;14:526–535.
Drossman DA. The role of psychosocial factors in gastrointestinal illness. Scand J Gastroenterol. 1996;221:1–4.
Duffy LC, Zielezny MA, Marshall JR, et al. Relevance of major stress events as an indicator of disease activity prevalence in 489 inflammatory bowel disease. Behav Med. 1991;17:101–110.
Casellas F, López-Vivancos J, Badiac X, et al. Impact of surgery for Crohn’s disease on health-related quality of life. Am J Gastroenterol. 2000;95:177–182.
Hjortswang H, Järnerot G, Curman B, et al. The influence of demographic and disease-related factors on health-related quality of life in patients with ulcerative colitis. Eur J Gastroenterol Hepatol. 2003;15:1011–1020.
Thirlby RC, Land JC, Fenster LF, et al. Effect of surgery on health-related quality of life in patients with inflammatory bowel disease: a prospective study. Arch Surg. 1998;133:826–832.
Cerveny P, Bortlík M, Kubena A, Vlcek J, Lakatos PL, Lukás M. Nonadherence in inflammatory bowel disease: results of factor analysis. Inflamm Bowel Dis. 2007;13:1244–1249.
Kane SV. Strategies to improve adherence and outcomes in patients with ulcerative colitis. Drugs. 2008;68:2601–2609.
Sajadinejad MS, Asgari K, Molavi H, Kalantari M, Adibi P. Psychological issues in inflammatory bowel disease: an overview. Gastroenterol Res Pract. 2012;2012:1–11. doi:10.1155/2012/106502.
Rowlinson A. Inflammatory bowel disease 3: importance of partnership in care. Br J Nurs. 1999;8:1013–1018.
Goldring AB, Taylor SE, Kemeny ME, Anton PA. Impact of health beliefs, quality of life, and the physician–patient relationship on the treatment intentions of inflammatory bowel disease patients. Health Psychol. 2002;21:219–228.
Nguyen GC, LaVeist TA, Harris ML, Datta LW, Bayless TM, Brant SR. Patient trust-in-physician and race are predictors of adherence to medical management in inflammatory bowel disease. Inflamm Bowel Dis. 2009;15:1233–1239.
Acknowledgments
We would like to thank Jayne Eaden, M.D., for her permission to use the CCKNOW.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Anilga Tabibian and James H. Tabibian are co-first authors.
Appendix
Appendix
Medical Outcomes Study General Adherence Items (MOS)
This questionnaire is about your tendency to follow doctor’s recommendations. Please circle one answer choice below.
How often was each of the following statements true for you during the past 4 weeks? (Circle one number on each line)
-
1.
I had a hard time doing what the doctor suggested I do…
-
(a)
None of the time
-
(b)
A little of the time
-
(c)
Some of the time
-
(d)
A good bit of the time
-
(e)
Most of the time
-
(f)
All of the time
-
(a)
-
2.
I followed my doctor’s suggestions exactly…
-
(a)
None of the time
-
(b)
A little of the time
-
(c)
Some of the time
-
(d)
A good bit of the time
-
(e)
Most of the time
-
(f)
All of the time
-
(a)
-
3.
I was unable to do what was necessary to follow my doctor’s treatment plans…
-
(a)
None of the time
-
(b)
A little of the time
-
(c)
Some of the time
-
(d)
A good bit of the time
-
(e)
Most of the time
-
(f)
All of the time
-
(a)
-
4.
I found it easy to do the things my doctor suggested I do
-
(a)
None of the time
-
(b)
A little of the time
-
(c)
Some of the time
-
(d)
A good bit of the time
-
(e)
Most of the time
-
(f)
All of the time
-
(a)
-
5.
Generally speaking, how often during the past 4 weeks were you able to do what the doctor told you?
-
(a)
None of the time
-
(b)
A little of the time
-
(c)
Some of the time
-
(d)
A good bit of the time
-
(e)
Most of the time
-
(f)
All of the time
-
(a)
Perceived Stress Scale-10 (PSS-10)
The questions in this scale ask you about your feelings and thoughts during the last month. In each case, you will be asked to indicate by circling how often you felt or thought a certain way.
0 = never 1 = almost never 2 = sometimes 3 = fairly often 4 = very often
1. In the last month, how often have you been upset because of something that happened unexpectedly? | 0 1 2 3 4 |
2. In the last month, how often have you felt that you were unable to control the important things in your life? | 0 1 2 3 4 |
3. In the last month, how often have you felt nervous and “stressed”? | 0 1 2 3 4 |
4. In the last month, how often have you felt confident about your ability to handle your personal problems? | 0 1 2 3 4 |
5. In the last month, how often have you felt that things were going your way? | 0 1 2 3 4 |
6. In the last month, how often have you found that you could not cope with all the things that you had to do? | 0 1 2 3 4 |
7. In the last month, how often have you been able to control irritations in your life? | 0 1 2 3 4 |
8. In the last month, how often have you felt that you were on top of things? | 0 1 2 3 4 |
9. In the last month, how often have you been angered because of things that were outside of your control? | 0 1 2 3 4 |
10. In the last month, how often have you felt difficulties were piling up so high that you could not overcome them? | 0 1 2 3 4 |
Rights and permissions
About this article
Cite this article
Tabibian, A., Tabibian, J.H., Beckman, L.J. et al. Predictors of Health-Related Quality of Life and Adherence in Crohn’s Disease and Ulcerative Colitis: Implications for Clinical Management. Dig Dis Sci 60, 1366–1374 (2015). https://doi.org/10.1007/s10620-014-3471-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-014-3471-1