Abstract
The aim of the present study was to evaluate the contribution of urate transporter genes and alcohol use to the risk of gout/tophi. Eight variants of ABCG2, SLC2A9, SLC22A12, SLC22A11 and SLC17A3 were genotyped in male individuals in a case–control study with 157 gout (33% tophi), 106 asymptomatic hyperuricaemia and 295 control subjects from Taiwan. The multilocus profiles of the genetic risk scores for urate gene variants were used to evaluate the risk of asymptomatic hyperuricaemia, gout and tophi. ABCG2 Q141K (T), SLC2A9 rs1014290 (A) and SLC22A12 rs475688 (C) under an additive model and alcohol use independently predicted the risk of gout (respective odds ratio for each factor=2.48, 2.03, 1.95 and 2.48). The additive composite Q141K, rs1014290 and rs475688 scores of high-risk alleles were associated with gout risk (P<0.0001). We observed the supramultiplicative interaction effect of genetic urate scores and alcohol use on gout and tophi risk (P for interaction=0.0452, 0.0033). The synergistic effect of genetic urate score 5–6 and alcohol use indicates that these combined factors correlate with gout and tophi occurrence.
Similar content being viewed by others
Introduction
Gout is a common type of inflammatory arthritis affecting 8.3 million people in the United States1 and 1.0 million people in Taiwan.2 Gout is characterised by hyperuricaemia and the intraarticular deposition of monosodium urate crystals.3 Most patients who develop gout have difficultly eliminating renal uric acid.4 Almost all of the circulating urate is filtered through the glomeruli, with typically only a small fraction (∼10%) of the uric acid excreted in the urine.5 Sustained hyperuricaemia, which is dysfunction in renal handling rather than reduced excretion of uric acid, is the dominant mechanism underlying the expansion of the urate pool.6 Uricase knockout mice possess serum urate levels of ∼10 mg dl−1. Uricase-deficient mice develop uric acid nephropathy, resulting in an approximately sixfold increase in urine volume and a fivefold increase in fluid requirements compared with normal mice, followed by death shortly before weaning.7 Humans, unlike most mammals, lack hepatic uricase because of mutational silencing.8 The absence of uricase combined with the extensive reabsorption of filtered urate results in human plasma urate levels ∼10 times those of most other mammals (30–59 μmol l−1).3, 9 Therefore, renal urate homeostasis is a critical determinant of systemic urate levels in the body.
The known risk factors for developing gout include hyperuricaemia, metabolic syndrome, renal disease, dietary factors, alcohol consumption, diuretic drug use and genetic factors.10 A number of mechanisms have been implicated in the pathogenesis of alcohol-induced hyperuricaemia that can increase or reduce the excretion of uric acid.6, 11, 12 Genome-wide association studies have identified several genes involved in the renal urate transport system that influence uric acid levels among various ethnic groups.13, 14, 15 A genome-wide association study of East Asian individuals identified ABCG2, SLC2A9 and SLC22A12 as urate transporter genes that are strongly associated with uric acid levels.15 Several variants within a number of genes responsible for excreting uric acid from the kidneys have been identified.16 Renal underexcretion and the activation of the inflammasome are known as important mechanisms of gout.3 Although genome-wide association studies employing large-scale samples have revealed novel susceptibility loci for uric acid levels, most studies have identified genes with small-to-moderate effects on hyperuricaemia and gout (effect size=1.1; odds ratio (OR)=2.4).17
In the present study, considering the polygenetic risk of hyperuricaemia and gouty arthritis, we hypothesised that the gout-susceptible hyperuricaemic gene variants of the physiological urate transporters in the renal proximal tubule epithelial cell could mediate interactions contributing to hyperuricaemia and gout as well as tophi risk. Thus, the aim of the present study was to estimate the genetic variants in the urate transporter genes that contribute to gout susceptibility in individuals who consume alcohol, and provide predictive biomarkers for gouty arthritis progression.
Materials and methods
Study participants
In a case–control study, a total of 558 Taiwanese Han men participated, including 295 controls with normal uric acid levels, 106 patients with asymptomatic hyperuricaemia and 157 gout patients (including 52 tophaceous gout patients). Gouty patients were diagnosed using criteria provided by the American College of Rheumatology18 and were examined for the presence of crystals as previously described that was confirmed at the rheumatology outpatient clinic.19, 20 Asymptomatic hyperuricaemia was defined as elevated serum urate concentration (exceeding 7.0 mg dl−1 in men) without symptoms or signs of monosodium urate crystal deposition disease (for example, gout) or uric acid renal disease. All controls had no history of gout and were not receiving antihyperuricemic drug for medical conditions. Information concerning drinking behaviour was collected through interviews using a questionnaire. Alcohol users were categorised into three groups: nondrinkers, former drinkers and current drinkers. Former drinkers were defined as individuals who had habitually consumed alcoholic beverages for more than 1 year but had stopped drinking. This study design was approved by the institutional review boards and ethics committees of the participating hospitals, and all participants provided written informed consent for the subsequent analyses.
Genotype determination
Venous whole blood was obtained from all participants, and DNA was extracted using standard extraction procedures (QIAGEN Gentra Puregene Blood Kit; Gentra Systems, Minneapolis, MN, USA). Most of the genes associated with serum uric acid levels or gout are involved in the renal urate transport system, including the urate transporter genes ABCG2, SLC2A9 and SLC22A12, that modulate serum uric acid levels and gout risk.16 The top-scoring polymorphism rs2231142 (Q141K) in ABCG2, which is involved in a major pathway for urate secretion in the proximal tubule, was selected,12 and two single-nucleotide polymorphisms (SNPs) within genes that are involved in a major pathway for urate reabsorption in the proximal tubule, namely SLC2A9 rs1014290 and SLC22A12 rs475688, were also included.21, 22 SLC17A3 rs116520512 and two SNPs, namely rs942379 S448S and rs1165165 A100T, within SLC17A3 (showing minor allele frequencies >10% according to HapMap–CHB), in addition to two SNPs within SLC22A11, namely rs693591 (a tag SNP common to both CEU and CHB that is associated with gout in New Zealanders)23 and rs1783811 (associated with torsemide renal clearance),24 were genotyped in this study. SLC22A11 rs2078267 (associated with gout in European Caucasians, with minor allele frequency=0.50)25, 26 was excluded from genotyping because this SNP is a rare variant in the 1000 Genomes–CHB Chinese samples (minor allele frequency <0.02). All SNPs were genotyped using TaqMan SNP Genotyping Assays on a 7900HT Fast Real-Time PCR System (Applied Biosystems, Foster City, CA, USA). All gene loci were genotyped without any sequence misses and subsequently used for all analyses.
Statistical analysis
Data handling and associations were performed using SAS software v.9.4 (SAS Institute, Cary, NC, USA). Hardy–Weinberg Equilibrium was verified for all SNPs using PLINK software v.1.07.27 The data for continuous and categorical variables were analysed using a general linear regression model (one-way analysis of variance) and the χ2 test. ORs with 95% confidence intervals (CIs) and P-values were determined using SNPs or using the additive, dominant or recessive models of inheritance after adjusting for age, body mass index, total cholesterol, triglycerides, creatinine, hypertension, alcohol use and every other SNP using a multinomial logistic regression model. Additive genetic effects were modelled by defining a continuous variable with levels 0, 1 and 2 (for example, T/T, C/T and C/C for rs475688; the C/C homozygous is a risk genotype for gout); the dominant or recessive effects were also calculated (for example, G/T+T/T versus G/G and T/T versus G/T+G/G for ABCG2 rs2231142 Q141K). Multifactor dimensionality reduction software was employed to calculate gene–gene and gene–environment interactions.28 A genetic risk score was generated after the number of risk alleles associated with gouty arthritis was counted (for Q141K (T), rs1014290 (A) and rs475688 (C), score range 0–6: Q141K T/T (score=2) + rs1014290 A/A (score=2) + rs475688 C/C (score=2)=6). The discriminative capability of the model was evaluated using logistic regression to generate C statistics. The sensitivity, specificity, positive predictive value, negative predictive value and accuracy by scores of 0–4 and 5–6 were calculated. The regression coefficient (β) represents changes to uric acid levels with changes in the genetic risk score after covariates were adjusted using a linear regression model. Partial η2 values were calculated as measures of variance in the genetic risk score in uric acid levels after covariates were adjusted using a general linear regression model. A multinomial logistic regression model, including genetic risk score × alcohol use interaction term, was applied after adjustment for covariates: model gout=genetic risk score + alcohol use + genetic risk score × alcohol + covariates. If clinical genetic testing was to be done, all individuals would be tested, and therefore we would be interested in the increased risk of genetic risk score 5–6 versus 0–4 on gout risk. Additive interactions were evaluated using a synergy index and corresponding 95% CIs, calculated29, 30 as (OR for genetic risk score 5–6 and alcohol use−1) ÷ ((OR for genetic risk score 5–6 + OR for alcohol use)−2), a SAS program using proc logistic to generate the input needed in the excel sheet after adjustment for covariates. The synergy index is a test of additive interaction that provides evidence that combined exposures are either superadditive (synergy index >1), compatible with additive (synergy index=1) or less than additive (synergy index <1). The attributable fraction (percentage) among all cases in the population (AF−Pop %) was estimated (exposure frequency in gout/tophi cases × (OR−1)/OR).31
Results
The baseline characteristics of the Taiwanese Han male study participants are shown in Table 1. Participants with gouty arthritis and asymptomatic hyperuricaemia had higher mean diastolic pressure, body mass index, total cholesterol, triglycerides, creatinine, uric acid and alcohol use as well as a greater proportion of comorbidity with hypertension (P<0.05).
We found that ABCG2 Q141K (T/T), SLC2A9 rs1014290 (A/A) and SLC22A12 rs475688 (C/C) were significantly associated with gout risk (prevalence proportion=31.2%, 52.2% and 44.6%, and OR=7.79, 5.05 and 3.43, respectively; Table 2). The results revealed that ABCG2 Q141K (T), SLC2A9 rs1014290 (A) and SLC22A12 rs475688 (C) under an additive model of inheritance remained independently associated with gout (OR=2.48, 2.03 and 1.95, and P=1.24 × 10−7, 9.53 × 10−5 and 1.45 × 10−4, respectively) and asymptomatic hyperuricaemia (only SLC2A9 rs1014290 (A); OR=1.62, P=6.26 × 10−3; Table 3). Our results also found that three SNPs under a dominant or recessive model were associated with gout (Tables 2 and 3). We observed a logistic regression model containing β-coefficient in each of genetic factors in Supplementary Table 1. We showed that the C-statistic was higher in additive model (0.75) than in the dominant and recessive models (0.68 and 0.72). Finally, three SNPs using an additive model would be evaluated. In addition, three SNPs of the β-coefficient under an additive model were <1, and hence we give ‘1’ score to each allele dose; the genetic risk score method (sum of the number of risk alleles) was equivalent to the β-coefficient score method.
No significant association was observed for SLC22A11 and SLC17A3 gene variants. Alcohol use (former drinkers) remained independently associated with gout (OR⩾2.48, P⩽0.0498), suggesting that the long-term effects of alcohol consumption affect the risk of gout. For multifactor dimensionality reduction, we combined two groups of former and current drinker for future analysis.
Next, we summarised these results according to the additive composite ABCG2, SLC2A9 and SLC22A12 scores of high-risk alleles, demonstrating that the incidence of hyperuricaemia and gout increased with genetic urate scores (Table 4). We found that the genetic risk scores of participants were widely distributed in the generic risk score range, with control participants and patients with asymptomatic hyperuricaemia and gout skewed to the lower and upper risk scores, respectively (P<0.0001). The C-statistic using the additive, dominant or recessive models with clinical factors was 0.85, 0.84 or 0.84. Similarly, for the model genetic risk score range or score 5–6 with clinical factors, the C-statistic was 0.85 or 0.83. As shown in Table 4, the sensitivity and specificity by scores of 5–6 and 0–4 were 28.7 and 92.9%; the positive predictive value and negative predictive value were 68.2 and 71.0%. The rule predicted gout with an accuracy of 70.6%.
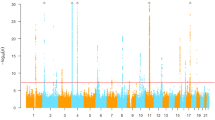
The genetic risk score for the partial η2 values (variance explained) of uric acid levels was 2.47% in controls after adjustment for covariates using a general linear regression model (β=0.11, P for trend=7.49 × 10−3; Figure 1). We also observed that the genetic risk score increment was associated with the risk of asymptomatic hyperuricaemia (1.33, 95% CI, 1.10–1.60, P=0.0030; Supplementary Table 2). Notably, we found the supramultiplicative interaction effect of adjustments in the value of the genetic risk scores and alcohol use on gout and tophi risk (Table 5). We revealed that genetic risk scores were associated with gout risk (OR=1.95 in alcohol nonusers and OR=2.92 in alcohol users) and that a genetic risk score × alcohol use interaction was associated with gout risk (P for interaction=0.0452). Consistently, in tophi gout patients, genetic risk scores were associated with risk (1.98 in alcohol nonusers and 7.09 in alcohol users), and genetic risk score × alcohol use interaction was associated with gouty tophi risk (P for interaction=0.0033). We suggest that alcohol intake might be modified when a genetic urate score demonstrates increased gout–tophi occurrence. Moreover, multifactor dimensionality reduction identified the interactions of Q141K, rs1014290 and rs475688 loci, resulting in a 14.01-fold (95% CI, 6.52–30.11) increase in the risk of tophi, and interactions among these three loci and alcohol use revealed up to a 28.05-fold (95% CI, 12.01–65.54) increase in the risk of tophi.
Genetic risk score of ABCG2 Q141K, SLC2A9 rs1014290 and SLC22A12 rs475688 contributed to uric acid levels in controls. Regression coefficient (β) with s.e. in parentheses represents the changes for uric acid levels with changes in the genetic risk score after adjustment for covariates using a linear regression model. The variance explained (partial η2) of uric acid levels in controls by this genetic risk score was 2.47% (effect size, β=0.11). Error bars indicate s.e.
To evaluate the contributions of individual genetic risk scores to disease progression, we classified the genetic risk scores as 0–4 and 5–6. Table 5 shows the joint effects of multilocus profiles of genetic risk scores and alcohol use in patients with gout and tophi. We found a significantly higher risk of gout and tophi in patients without alcohol use and a genetic risk score of 5–6 (OR=3.98, 3.81 and P=3.10 × 10−4, 0.0141), and with a genetic risk score of 5–6 with alcohol use (OR=17.84, 50.65; P=1.71 × 10−5, 5.51 × 10−8; synergy index=5.36, 15.99, respectively), suggesting a positive superadditive interaction between urate transporter gene variants and alcohol use. Moreover, the relatively high incidence of gout and tophi in participants with a genetic risk score of 5–6 (15.9% and 13.5%, respectively, vs 6.1% among controls) and with joint exposure (12.7% and 26.9%, respectively, vs 1.0% among controls) indicates considerable population-attributable fractions for gout and tophi (11.9 and 12.0% in gout patients; 10.0 and 26.4% in tophi patients; Supplementary Figure 1).
Discussion
The present study represented a step towards elucidating the effects of gout-susceptible hyperuricaemic gene variants on gout risk and gaining a broader understanding of tophaceous gout development. Higher genetic scores for the high-risk alleles of the three genes examined were associated with asymptomatic hyperuricaemia, gout and tophaceous gout. Notably, we demonstrated the supramultiplicative effect of genetic risk scores combined with alcohol use regarding gout and tophi risk (OR=2.92, 7.09; P for interaction=0.0452, 0.0033). For clinical genetic testing, we distinguished between the increased risk in those with a 5–6 score vs the increased risk in those with a 0–4 gout risk group score. We identified a superadditive interaction effect in the 5–6 genetic risk score group with alcohol use for gout and tophi risk (OR=17.84, 50.65; P=1.71 × 10−5, 5.51 × 10−8). The attributable fractions of gout and tophi explained by joint exposure (5–6 score with alcohol use) were 12.0% and 26%, respectively. This study illustrated that an additive composite genetic urate score for high-risk allele testing and alcohol use assessment should be applied in integrative care for patients with gout.
Most patients who develop gout have difficulty eliminating renal uric acid,4 and therefore, the mechanisms responsible for urate transport in the kidneys have considerable clinical value. ABCG2 is a well-studied hyperuricaemic gene that encodes a secretory urate transporter in the kidneys.16 Cytokines and growth factors have been implicated in the regulation of ABCG2 gene expression.32 SLC2A9 (4p16.1) is a high-capacity uric acid transporter that is expressed in renal epithelial cells, hepatocytes, peripheral leukocytes and articular cartilage.13, 16 SLC22A12 variants have been associated with uric acid levels and reduced fractional urate excretion that accounts for most hyperuricaemia and gout cases.15, 16 SLC2A9, similar to SLC22A12, is a uric acid transporter that can be inhibited using a uricosuric agent (benzbromarone)33 (for example, uricosuric drugs targeting SLC2A9/SLC22A12 in gout to prevent the reuptake of uric acid, thereby increasing renal urate excretion). The urate transporter genes ABCG2, SLC2A9 and SLC22A12 modulate serum uric acid levels and gout risk.16
Dehghan et al.12 reported that genetic risk scores for ABCG2 rs2231142 Q141K, SLC2A9 rs16890979 V253I and SLC17A3 rs1165205 are associated with increased uric acid concentrations and gout in Caucasians. They further identified substantial associations between a missense SLC2A9 rs16890979 V253I variant or the SLC17A3 rs1165205 polymorphism and gout; however, this effect was not observed in African-American participants.12 Although the V253I variant confers a similar risk for gout in Māori, Pacific Islanders and New Zealanders (Caucasian),34 V253I is a rare variant in HapMap–CHB Chinese samples (minor allele frequency <0.01). In the present study, we observed no significant association between SLC17A3 rs1165205 with hyperuricaemia and gout. The most significant association between SLC2A9 and low fractional excretion of uric acid and gout involved the SNP rs1014290 in German and Scottish cohorts.13 We demonstrated that only SLC2A9 rs1014290 was associated with asymptomatic hyperuricaemia (OR=1.62, P=6.26 × 10−3). Furthermore, we provided evidence for an association between SLC2A9 rs1014290 with gout and tophaceous gout in Taiwanese Han people.22 We found that mean uric acid concentrations increased linearly with increasing uric acid risk by 0.11 mg dl−1 (P-trend=7.49 × 10−3), and each additional copy of a risk allele was associated with an increased asymptomatic hyperuricaemia risk (OR=1.33, P=0.0030; Supplementary Table 2). We suggest that the SLC2A9 gene could be a crucial genetic checkpoint for hyperuricaemia, gout and tophi development. Several associations between SLC22A12 variants, serum uric acid concentrations and gout have been reported (for example, rs475688 in European Caucasians and Taiwanese Han people).16, 23 Herein this study differs from previous studies,20, 21, 22 as our findings revealed that the multilocus profiles of ABCG2, SLC2A9 and SLC22A12 are associated with urate levels (P-trend=7.49 × 10−3), gout risk (genetic risk score × alcohol use, P for interaction=0.0452) and especially tophi risk (P for interaction=0.0033) in Taiwanese Han people.
Gout is a complex disease that is associated with multiple genetic and environmental factors. Alcohol has been recognised as a potential risk factor for gout and is considered a trigger for acute gouty arthritis and recurrent gout attacks.35, 36 A number of mechanisms have been implicated in the pathogenesis of alcohol-induced hyperuricaemia because alcohol directly affects urate transporters in the kidneys and increases or reduces the excretion of uric acid.6, 36, 37 In the present study, we revealed that the joint effects of a genetic risk score of 5–6 and alcohol use result in severe gout risk (OR=50.53, P for interaction=0.0137, genetic risk score of 5–6 × alcohol use interaction), indicating considerable population-attributable fractions for tophi (from 12.0 to 26.4%). The combined effects of high-risk allele urate scores and alcohol use in modulating tophaceous gout risk may be more pronounced than the mere summation of the individual risk resulting from genetic risk scores or alcohol use.
The factors determining the development of tophi remain unknown. Sodium urate monohydrate crystals act as endogenous danger signals, generating adaptive, nonmicrobial innate immunity.38 For those with urate levels of ⩾9.0 mg dl−1, the cumulative incidence of gouty arthritis is 22% after 5 years;39 tophaceous gout develops within 5 years of gout onset in 30% of untreated patients.40 Thus, different immune responses to monosodium urate crystals might result in different manifestations of the disease (for example, nontophaceous gout and tophaceous gout).34 In addition, almost all of the circulating urate is filtered through glomeruli, with only a small fraction (∼10% of the uric acid) typically excreted in urine.5 Notably, only a minority (20%) of hyperuricaemic individuals experience gout clinical symptoms.6 In this study, we observed that individual common genetic variants (risk-homozygous genotype frequencies 31.2–52.2%; Table 2) confer a modest risk of gout. We also showed that the combination of these variants is markedly associated with the development and progression of tophaceous gout. Therefore, the multilocus profiles of genetic risk scores could be differentially associated with gout complications, particularly joint destruction or deformity, or poor response to drugs.
The present proof-of-principle paper demonstrates that the multilocus profiles of ABCG2, SLC2A9 and SLC22A12 increase susceptibility to asymptomatic hyperuricaemia, gout and tophi. This paper also reveals the supramultiplicative interaction effect of genetic urate scores and alcohol use on gout and tophi risk. This information could help identify individuals at risk for asymptomatic hyperuricaemia and gout (in particular, severe gout development) long before the onset of clinical symptoms of the disease. These findings might assist in the counselling of gout-susceptible individuals and alcohol users. In addition to risk prediction, the genotype or risk score for a hyperuricaemic individual could be used to recommend lifestyle adjustments such as low alcohol consumption and a low purine diet to reduce the risk of developing gout and may further ameliorate the disease courses of patients with established gout, considering that early risk stratification could minimise the need for long-term therapy and associated costs.
References
Zhu, Y., Pandya, B. J. & Choi, H. K. Prevalence of gout and hyperuricemia in the US general population: the National Health and Nutrition Examination Survey 2007-2008. Arthritis Rheum. 63, 3136–3141 (2011).
Kuo, C. F., Grainge, M. J., See, L. C., Yu, K. H., Luo, S. F., Valdes, A. M. et al. Familial aggregation of gout and relative genetic and environmental contributions: a nationwide population study in Taiwan. Ann. Rheum. Dis. 74, 369–374 (2015).
Choi, H. K., Mount, D. B. & Reginato, A. M. Pathogenesis of gout. Ann. Intern. Med. 143, 499–516 (2005).
Aringer, M. & Graessler, J. Understanding deficient elimination of uric acid. Lancet 372, 1929–1930 (2008).
Terkeltaub, R. Update on gout: new therapeutic strategies and options. Nat. Rev. Rheumatol. 6, 30–38 (2010).
Hediger, M. A., Johnson, R. J., Miyazaki, H. & Endou, H. Molecular physiology of urate transport. Physiology (Bethesda) 20, 125–133 (2005).
Kelly, S. J., Delnomdedieu, M., Oliverio, M. I., Williams, L. D., Saifer, M. G., Sherman, M. R. et al. Diabetes insipidus in uricase-deficient mice: a model for evaluating therapy with poly(ethylene glycol)-modified uricase. J. Am. Soc. Nephrol. 12, 1001–1009 (2001).
Wu, X. W., Lee, C. C., Muzny, D. M. & Caskey, C. T. Urate oxidase: primary structure and evolutionary implications. Proc. Natl Acad. Sci. USA 86, 9412–9416 (1989).
Wu, X. W., Muzny, D. M., Lee, C. C. & Caskey, C. T. Two independent mutational events in the loss of urate oxidase during hominoid evolution. J. Mol. Evol. 34, 78–84 (1992).
Saag, K.G. & Choi, H. Epidemiology, risk factors, and lifestyle modifications for gout. Arthritis Res. Ther. 8 (suppl. 1), S2 (2006).
Eraly, S. A., Vallon, V., Rieg, T., Gangoiti, J. A., Wikoff, W. R., Siuzdak, G. et al. Multiple organic anion transporters contribute to net renal excretion of uric acid. Physiol. Genomics 33, 180–192 (2008).
Dehghan, A., Kottgen, A., Yang, Q., Hwang, S. J., Kao, W. L., Rivadeneira, F. et al. Association of three genetic loci with uric acid concentration and risk of gout: a genome-wide association study. Lancet 372, 1953–1961 (2008).
Vitart, V., Rudan, I., Hayward, C., Gray, N. K., Floyd, J., Palmer, C. N. et al. SLC2A9 is a newly identified urate transporter influencing serum urate concentration, urate excretion and gout. Nat. Genet. 40, 437–442 (2008).
Kolz, M., Johnson, T., Sanna, S., Teumer, A., Vitart, V., Perola, M. et al. Meta-analysis of 28,141 individuals identifies common variants within five new loci that influence uric acid concentrations. PLoS Genet. 5, e1000504 (2009).
Okada, Y., Sim, X., Go, M. J., Wu, J. Y., Gu, D., Takeuchi, F. et al. Meta-analysis identifies multiple loci associated with kidney function-related traits in east Asian populations. Nat. Genet. 44, 904–909 (2012).
Reginato, A. M., Mount, D. B., Yang, I. & Choi, H. K. The genetics of hyperuricaemia and gout. Nat. Rev. Rheumatol. 8, 610–621 (2012).
Merriman, T. R. & Dalbeth, N. The genetic basis of hyperuricaemia and gout. Joint Bone Spine 78, 35–40 (2011).
Wallace, S. L., Robinson, H., Masi, A. T., Decker, J. L., McCarty, D. J. & Yu, T. F. Preliminary criteria for the classification of the acute arthritis of primary gout. Arthritis Rheum. 20, 895–900 (1977).
Ko, A. M., Tu, H. P., Liu, T. T., Chang, J. G., Yuo, C. Y., Chiang, S. L. et al. ALPK1 genetic regulation and risk in relation to gout. Int. J. Epidemiol. 42, 466–474 (2013).
Tu, H. P., Ko, A. M., Chiang, S. L., Lee, S. S., Lai, H. M., Chung, C. M. et al. Joint effects of alcohol consumption and ABCG2 Q141K on chronic tophaceous gout risk. J. Rheumatol. 41, 749–758 (2014).
Tu, H. P., Chen, C. J., Lee, C. H., Tovosia, S., Ko, A. M., Wang, S. J. et al. The SLC22A12 gene is associated with gout in Han Chinese and Solomon Islanders. Ann. Rheum. Dis. 69, 1252–1254 (2010).
Tu, H. P., Chen, C. J., Tovosia, S., Ko, A. M., Lee, C. H., Ou, T. T. et al. Associations of a non-synonymous variant in SLC2A9 with gouty arthritis and uric acid levels in Han Chinese subjects and Solomon Islanders. Ann. Rheum. Dis. 69, 887–890 (2010).
Flynn, T. J., Phipps-Green, A., Hollis-Moffatt, J. E., Merriman, M. E., Topless, R., Montgomery, G. et al. Association analysis of the SLC22A11 (organic anion transporter 4) and SLC22A12 (urate transporter 1) urate transporter locus with gout in New Zealand case-control sample sets reveals multiple ancestral-specific effects. Arthritis Res. Ther. 15, R220 (2013).
Vormfelde, S. V., Schirmer, M., Hagos, Y., Toliat, M. R., Engelhardt, S., Meineke, I. et al. Torsemide renal clearance and genetic variation in luminal and basolateral organic anion transporters. Br. J. Clin. Pharmacol. 62, 323–335 (2006).
Yang, Q., Kottgen, A., Dehghan, A., Smith, A. V., Glazer, N. L., Chen, M. H. et al. Multiple genetic loci influence serum urate levels and their relationship with gout and cardiovascular disease risk factors. Circ. Cardiovasc. Genet. 3, 523–530 (2010).
Kottgen, A., Albrecht, E., Teumer, A., Vitart, V., Krumsiek, J., Hundertmark, C. et al. Genome-wide association analyses identify 18 new loci associated with serum urate concentrations. Nat. Genet. 45, 145–154 (2013).
Purcell, S., Neale, B., Todd-Brown, K., Thomas, L., Ferreira, M. A., Bender, D. et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am. J. Hum. Genet. 81, 559–575 (2007).
Ritchie, M. D. & Motsinger, A. A. Multifactor dimensionality reduction for detecting gene-gene and gene-environment interactions in pharmacogenomics studies. Pharmacogenomics 6, 823–834 (2005).
Hosmer, D. W. & Lemeshow, S. Confidence interval estimation of interaction. Epidemiology 3, 452–456 (1992).
Andersson, T., Alfredsson, L., Kallberg, H., Zdravkovic, S. & Ahlbom, A. Calculating measures of biological interaction. Eur. J. Epidemiol. 20, 575–579 (2005).
Botto, L. D. & Khoury, M. J. Commentary: facing the challenge of gene-environment interaction: the two-by-four table and beyond. Am. J. Epidemiol. 153, 1016–1020 (2001).
Robey, R. W., To, K. K., Polgar, O., Dohse, M., Fetsch, P., Dean, M. et al. ABCG2: a perspective. Adv. Drug Deliv. Rev. 61, 3–13 (2009).
Enomoto, A., Kimura, H., Chairoungdua, A., Shigeta, Y., Jutabha, P., Cha, S. H. et al. Molecular identification of a renal urate anion exchanger that regulates blood urate levels. Nature 417, 447–452 (2002).
Hollis-Moffatt, J. E., Gow, P. J., Harrison, A. A., Highton, J., Jones, P. B., Stamp, L. K. et al. The SLC2A9 nonsynonymous Arg265His variant and gout: evidence for a population-specific effect on severity. Arthritis Res. Ther. 13, R85 (2011).
Neogi, T., Chen, C., Niu, J., Chaisson, C., Hunter, D. J. & Zhang, Y. Alcohol quantity and type on risk of recurrent gout attacks: an internet-based case-crossover study. Am. J. Med. 127, 311–318 (2014).
Choi, H. K., Atkinson, K., Karlson, E. W., Willett, W. & Curhan, G. Alcohol intake and risk of incident gout in men: a prospective study. Lancet 363, 1277–1281 (2004).
Faller, J. & Fox, I. H. Ethanol-induced hyperuricemia: evidence for increased urate production by activation of adenine nucleotide turnover. N. Engl. J. Med. 307, 1598–1602 (1982).
Dalbeth, N. & Merriman, T. Crystal ball gazing: new therapeutic targets for hyperuricaemia and gout. Rheumatology (Oxford) 48, 222–226 (2009).
Campion, E. W., Glynn, R. J. & DeLabry, L. O. Asymptomatic hyperuricemia. Risks and consequences in the Normative Aging Study. Am. J. Med. 82, 421–426 (1987).
Richette, P. & Bardin, T. Gout. Lancet 375, 318–328 (2010).
Acknowledgements
This work was supported by grants from the Ministry of Science and Technology (MOST-104–2632-B-039–001 and MOST 104–2314-B-037–036) and China Medical University (CMU 104-S-22, 25, 26, 28), Taiwan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Journal of Human Genetics website
Rights and permissions
About this article
Cite this article
Tu, HP., Chung, CM., Min-Shan Ko, A. et al. Additive composite ABCG2, SLC2A9 and SLC22A12 scores of high-risk alleles with alcohol use modulate gout risk. J Hum Genet 61, 803–810 (2016). https://doi.org/10.1038/jhg.2016.57
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2016.57
This article is cited by
-
The association between genetic polymorphisms in ABCG2 and SLC2A9 and urate: an updated systematic review and meta-analysis
BMC Medical Genetics (2020)
-
The association between genotypes of urate transporter-1, Serum uric acid, and mortality in the community-based population: the Yamagata (Takahata) Study
Clinical and Experimental Nephrology (2019)
-
Risk of incident benign prostatic hyperplasia in patients with gout: a retrospective cohort study
Prostate Cancer and Prostatic Diseases (2018)
-
Variants of ALPK1 with ABCG2, SLC2A9, and SLC22A12 increased the positive predictive value for gout
Journal of Human Genetics (2018)
-
The genetics of gout: towards personalised medicine?
BMC Medicine (2017)