Key Points
-
Epitope spreading is defined as the diversification of epitope specificity from the initial focused, dominant epitope-specific immune response, directed against a self or foreign protein, to subdominant and/or cryptic epitopes on that protein (intramolecular spreading) or other proteins (intermolecular spreading).
-
The immune response consists of an initial magnification phase, which can either be deleterious as in autoimmune disease or beneficial as in vaccinations, and a later downregulatory phase to return the immune system to homeostasis. Epitope spreading may be an important component of both phases.
-
Human studies strongly suggest that epitope spreading has a role in ongoing disease, although epitope spreading is very difficult to verify in human disease. Animal models have therefore been useful, as the peptide specificity of the initial immune response can be manipulated, genetically identical animals used, and the immune response over time in different lymphoid organs and in the target tissue can be assessed.
-
Studies in two models of multiple sclerosis, experimental autoimmune encephalomyelitis (EAE) and Theiler's murine encephalitogenic virus-induced demyelinating disease (TMEV-IDD) have shown conclusively that epitope spreading plays a pathological role in ongoing disease and that blocking this process by inducing tolerance to spread myelin epitopes or blocking costimulation of T cells (necessary for epitope spreading) blocks (EAE) or inhibits (TMEV-IDD) ongoing clinical disease.
-
Early tolerance to glutamic acid decarboxylase (GAD) in the non-obese diabetic (NOD) mouse model of diabetes has been shown to block epitope spreading and disease progression. Several human studies have observed epitope spreading in beta cell-specific humoral responses from birth to disease onset in offspring of diabetic parents.
-
Convincing evidence for the pathological role of epitope spreading is also seen in experimental autoimmune myasthenia gravis (EAMG) and adjuvant arthritis. Epitope spreading might also play a role in chronic graft rejection.
-
Treatment of human autoimmune diseases must take into consideration the dynamic nature of both the magnification and downregulatory phases of the immune response. With knowledge of the initial immune target, early antigen-specific treatments can block continued tissue damage, epitope spreading and clinical disease.
-
Induction of anti-inflammatory T helper (TH)2 responses via epitope spreading may be an important intrinsic immunoregulatory mechanism geared to limit tissue destruction and promote re-establishment of tissue-specific immune tolerance.
-
Early induction of a TH2 response to one specific β-cell autoantigen (βCAA) accelerated epitope spreading of TH2 responses to other βCAAs and can prevent the development of diabetes in the NOD mice.
-
Tumour vaccination studies suggest that epitope spreading may increase the efficiency of peptide vaccination.
Abstract
Evidence continues to accumulate supporting the hypothesis that tissue damage during an immune response can lead to the priming of self-reactive T and/or B lymphocytes, regardless of the specificity of the initial insult. This review will focus primarily on epitope spreading at the T-cell level. Understanding the cellular and molecular basis of epitope spreading in various chronic immune-mediated human diseases and their animal models is crucial to understanding the pathogenesis of these diseases and to the ultimate goal of designing antigen-specific treatments.
Similar content being viewed by others
Main
A typical immune response against a self or foreign protein is usually focused on one or two epitopes within that protein, which are termed dominant. Epitope spreading was initially defined as the diversification of epitope specificity from the initial focused, dominant epitope-specific immune response to subdominant epitopes on that protein1,2. The hierarchy of dominant and CRYPTIC EPITOPES in this scenario is thought to be due to a combination of differential protein processing and presentation by various antigen-presenting cell populations, and also to the availability of epitope-specific T cells, taking into consideration central and peripheral tolerance mechanisms3.
Our laboratory and others, extending this view, have studied epitope spreading specifically in the context of chronic tissue damage, which can lead to autoimmunity. In these studies, regardless of the initial antigenic stimulus — be it viral, graft rejection or autoimmune — the specificity of the immune response spreads to include self epitopes other than that which initiated the inflammatory process (Fig. 1). In this scenario, infection, organ transplantation or autoimmunity (organ-specific or systemic) leads to tissue damage. The resulting inflammation and tissue damage then primes a hierarchical cascade of autoreactive T-cell specificities, even allowing cryptic or sequestered epitopes to be processed and presented.
Presentation of the primary epitope (the immunodominant self or viral epitope) occurs in peripheral lymphoid tissue (a), resulting in activation and differentiation of autoreactive TH1 cells (b). The activated TH1 cells migrate (c) into the target tissue, where they encounter antigen presented by resident APCs. (d). After antigen restimulation, the pathologic TH1 cells release a cascade of chemokines and cytokines (e), leading to recruitment of additional mononuclear phagocytes from the peripheral blood, which are activated along with resident APCs (f). Activated mononuclear cells then lead to bystander tissue destruction (g) via phagocytic mechanisms and release of TNF-α, proteolytic enzymes, NO and O2 radicals. The tissue debris (h) is processed and presented on resident and peripheral APCs (i), leading to the activation and differentiation of a second wave of TH1 cells (j), which can re-enter the tissue and cause additional tissue destruction. APC, antigen presenting cell; IFN-γ, interferon-γ; LT/TNF-β, lymphotoxin/tumour necrosis factor β; MIP-1α, macrophage inflammatory protein 1α; MHC II, major histocompatibility complex class II; Mono, monocyte; TCR, T-cell receptor; TH1, T helper cells type 1 (see glossary).
In most of the models to be discussed, epitope spreading initiated as a result of tissue damage is thought to play an active role in ongoing disease pathology. However, there is some evidence that epitope spreading is an important component of protective immune responses, acting to enhance the efficiency of the immune response, as seen in tumour clearance, and as a mechanism to downregulate immune responses, such as those occurring in autoimmunity.
At present, most treatment regimens for autoimmune diseases like multiple sclerosis, type-1 diabetes and myasthenia gravis rely on generalized suppression of the immune system and/or neutralization of inflammatory mediators. It is, however, desirable to design antigen-specific forms of immunotherapy that leave the immune system intact and able to neutralize opportunistic pathogens. Mounting evidence for a pathological role for epitope spreading in chronic autoimmune disease makes the development of epitope-specific therapies problematic4. Therefore, a more complete understanding of the cellular and molecular basis of the epitope spreading phenomenon is required to promote the development of antigen-specific treatments for human autoimmune diseases, more efficient vaccines and more effective methods to control transplant rejection.
Epitope spreading in autoimmune disease
Characterization of the cellular and molecular basis of epitope spreading in various chronic immune-mediated diseases and disease models is extremely important both to understanding the pathogenesis of those diseases and to achieving the ultimate goal of designing antigen-specific treatments for human autoimmune diseases. Although immune responses are complex, involving both humoral and cellular immune components, some autoimmune diseases are predominately CD4+ T-cell mediated, whereas others seem to be primarily antibody mediated. We will focus on the role of epitope spreading in T-cell-mediated autoimmune diseases. Although we present some intriguing human studies, a pathological role for epitope spreading is very difficult to verify in human disease because the initiating antigenic specificity is usually impossible to define. Animal models have therefore been useful because the peptide specificity of the initial immune response can be manipulated, genetically identical animals can be used and the immune response can be serially assessed in different peripheral lymphoid organs, as well as in the target tissue of the disease.
Autoimmune models of multiple sclerosis. Multiple sclerosis is a human autoimmune demyelinating disease thought to be CD4+ T-cell mediated and to be characterized by mononuclear cell infiltration into the central nervous system (CNS). Autoimmune and virus-induced animal models of multiple sclerosis have yielded many insights into the possible mechanisms involved in the human disease. The study of experimental autoimmune encephalomyelitis (EAE), which is induced by priming the animal with myelin antigens — including myelin basic protein (MBP), proteolipid protein (PLP), myelin oligodendrocyte glycoprotein (MOG) and myelin peptides — led to the initial description of epitope spreading1,2. EAE has been an excellent model in which to study this process because in this model disease is easily induced by a defined peptide, and the changing specificity of the immune response to endogenous myelin epitopes after disease initiation and subsequent tissue damage can be followed over time. In addition, EAE presents as either an acute, relapsing–remitting or chronic disease (as does multiple sclerosis), depending on the mouse strain used and the priming myelin epitopes (Table 1). Multiple investigators have characterized a hierarchical order of epitope spreading in various EAE systems and have shown a pathological role for this process in chronic disease progression3,5,6,7,8,9.
Our laboratory has extensively characterized the role of epitope spreading in relapsing EAE initiated by priming SJL mice with the immunodominant PLP epitope, PLP139–151. In this model, PLP139–151-specific CD4+ T-cell reactivity is induced within 3 days of priming and is maintained throughout the disease course. Immediately before, and continuing during, the first relapse, PLP178–191 reactivity (INTRAMOLECULAR EPITOPE SPREADING) is detected by T-cell proliferation and delayed-type hypersensitivity (DTH) assays, and during the second relapse, MBP84–104 responses (INTERMOLECULAR EPITOPE SPREADING) are identified (Fig. 2a). The development of these responses has been shown to correlate with the extent of myelin destruction during the acute disease phase, and T cells isolated from the CNS of sick mice proliferate to the spread epitopes PLP178–191 and MBP84–104. These T cells can also transfer disease to naive recipients9. More convincingly, peptide-specific tolerance to the relapse-associated epitopes blocks disease progression, even though peripheral T-cell responses against the disease-inducing peptide PLP139–151 remain intact10. For example, PLP178–191-specific tolerance induction during remission from PLP139–151-induced EAE reduced the relapse incidence from 80% in controls to 20% in tolerant mice.
a | The relapsing–remitting clinical course and pattern of epitope spreading in relapsing-EAE in the SJL mouse induced by priming with the immunodominant PLP139–151 epitope. Acute disease is mediated by PLP139–151-specific TH1 cells, which are then downregulated, resulting in disease remission. Myelin destruction during the acute clinical episode leads to the priming of T cells to a secondary epitope, PLP178–191 (intramolecular epitope spreading), which mediates the primary relapse. After regulation of these cells, a third wave of TH1 cells is induced to the lesser immunodominant MBP84–104 epitope (intermolecular epitope spreading), which mediates the secondary relapse. b | The clinical course and pattern of epitope spreading in TMEV-IDD in the SJL mouse. Disease onset is initiated by TMEV-specific CD4+ T cells, which arise several days after intracerebral infection and release proinflammatory cytokines upon encountering virus epitopes presented by persistently infected antigen-presenting cells in the CNS. These virus-specific responses persist throughout the chronic disease course. Myelin debris released as a result of the initial tissue damage leads to the induction of CD4+ TH1 responses against myelin epitopes, which occurs in a hierarchical order, beginning with responses to the immunodominant PLP139–151 epitope and then progressing to less-dominant myelin epitopes. MBP, myelin basic protein; MOG, myelin oligodendrocyte glycoprotein; PLP, proteolipid protein; TMEV, Theiler's murine encephalomyelitis virus.
It is also interesting that the hierarchical order of epitope spreading during relapsing EAE in the SJL mouse correlates with the size of the T-cell repertoire, with the pattern of spreading proceeding from the most to the least immunodominant epitope (that is, PLP139–151>PLP178–191>MBP84–104)10. In the SJL mouse, it has long been known that the response to the PLP139–151 epitope is dominant in EAE induced by mouse spinal cord homogenate11. This is in agreement with recent findings of a very high precursor frequency of PLP139–151-reactive T cells in the periphery of naive SJL mice. This high precursor frequency is partly due to lack of thymic deletion to PLP139–151, because an alternative isoform of PLP (DM20, which lacks residues 116–150) is more abundantly expressed in the thymus than is full-length PLP12. Even though other encephalitogenic epitopes such as PLP178–191 and MBP84–104 bind the SJL major histocompatibility complex (MHC) class II molecule with efficiency close to that of PLP139–151, induction of EAE with any myelin epitope other than PLP139–151 invariably leads to spreading first to PLP139–151-specific T cells9,10.
Some circumstantial evidence that epitope spreading occurs in human autoimmune disease is presented later in this review. If epitope spreading proves to be an integral part of chronic human autoimmune disease, peptide-specific therapies may be problematic, as the specificity of the pathogenic response would change over time. However, full T-cell activation, and therefore functional epitope spreading, requires co-stimulatory signals such as those provided by CD28–CD80/86 and CD154–CD40 interactions. In this regard, short-term blockade of CD28–CD80 co-stimulation using anti-CD80 F(ab) fragments administered after recovery from acute PLP139–151-induced relapsing EAE resulted in a striking reduction in relapse incidence13. This protection was long lasting, and worked efficiently even when treatment began after the first relapse. Importantly, CD28 blockade seemed to lead to specific tolerance of T-cell responses to the relapse-associated PLP178–191 epitope10. For example, when administered before the first relapse, anti-CD80 F(ab) therapy resulted in PLP178–191-specific tolerance and protection from disease relapse, even though peripheral T HELPER TYPE 1 (TH1) responses to the initiating PLP139–151 epitope were unaffected. Similarly, we have shown that short-term blockade of the CD40–CD154 interaction using a monoclonal anti-CD154 antibody administered either at the peak of acute disease, or during remission from acute disease, significantly inhibited disease relapse concomitant with suppression of T-cell reactivity to the relapse-associated myelin epitopes14. These results indicate that epitope spreading plays a major role in EAE progression in SJL mice, and short term co-stimulatory blockade can specifically inhibit initiation of T-cell responses to the spread epitope and expression of clinical relapses. Interestingly, treatment of SJL mice during ongoing relapsing EAE using intact antibodies or F(ab) fragments specific for the downregulatory co-stimulatory molecule cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) led to exacerbated disease progression and enhanced T-cell reactivity to both inducing and relapse-associated epitopes15,16. This indicates that normally, CTLA-4-mediated signalling negatively regulates the dynamic spread of autoreactive T-cell responses during the course of autoimmune disease.
Relapsing EAE induced in (SWR×SJL)F1 mice has also been extensively characterized. The immune response to the inducing peptide PLP139–151 declines with time, whereas responses to new myelin epitopes emerge5,17. Interestingly, interferon-β (IFN-β) treatment, which reduces disease relapses in these mice and in multiple sclerosis patients18,19, inhibits epitope spreading in the mouse model20. Responses to PLP139–151 after IFN-β treatment are essentially unchanged, with one important exception. Splenocytes from mice treated with IFN-β and activated ex vivo with PLP139–151 produced significantly more interleukin-10 (IL-10) and less IL-12 than control mice, indicating that IFN-β may reduce the relapse rate by creating a TH2-like environment in which epitope spreading is blocked20. IL-10 inhibits expression of proinflammatory cytokines21,22, MHC class II molecules23 and co-stimulatory24 molecules by antigen-presenting cells (APCs). These properties would probably limit tissue destruction and the ability of APCs to activate T cells that are specific to new antigens; that is, epitope spreading.
Epitope spreading has also been described by McFarland et al. in the nonhuman primate (marmoset) MP4-induced EAE model. MP4 is a fusion protein consisting of PLP and MBP. In this model, demyelination was found to be associated with a humoral response to MOG, a myelin protein not included in the inducing MP4 fusion protein25.
Although more difficult to prove, there is evidence that epitope spreading occurs in human multiple sclerosis. Recently, Tuohy et al. followed T-cell responses over several years in three IMDS (ISOLATED MONOSYMPTOMATIC DEMYELINATING SYNDROME) patients, showing that T-cell autoreactivity to particular PLP epitopes decreased with time after diagnosis. Interestingly, when two of these patients progressed to clinically definite multiple sclerosis, autoreactivity to PLP peptides other than those first observed appeared17,26,27. Goebeles et al. studied five multiple sclerosis patients by isolating MBP-specific T-cell lines at five time points. Specificity was determined using a panel of overlapping peptides and repertoire analysis was done by TCR Vβ CDR3 SPECTRATYPING. It was concluded that a pattern of a focused, stable epitope response is the exception rather than the rule in progressive multiple sclerosis28.
Virally induced models of multiple sclerosis. Viruses and other infectious insults are implicated in the aetiology of many human autoimmune diseases, including multiple sclerosis29. There are various mechanisms by which infection can lead to the initiation of an autoimmune response. These include molecular mimicry, bystander activation, release of cryptic epitopes and epitope spreading (Fig. 3). Spreading from viral to self epitopes has been shown or suggested to play a pathological role in several virus-induced autoimmune disease models, whereas bystander activation and molecular mimicry are thought to be involved in other diseases (reviewed in Ref. 30) (Table 2). We have examined the role of epitope spreading in initiating anti-myelin autoimmune responses in the chronic stages of Theiler's murine encephalitogenic virus-induced demyelinating disease (TMEV-IDD). TMEV, a picornavirus and natural mouse pathogen, induces a life-long persistent infection of CNS-resident APCs, leading to a chronic–progressive CD4+ T-cell-mediated demyelinating disease in susceptible mouse strains such as SJL/J. Myelin destruction is initiated by virus-specific CD4+ T cells, which target CNS-persistent virus31. Peripheral T-cell responses to myelin epitopes develop during progressive disease in a hierarchical order, beginning with the dominant PLP139–151 peptide (Fig. 2b), but only after the onset of demyelination32,33. As disease progresses, responses to various other less-dominant encephalitogenic myelin epitopes (such as PLP178–191, PLP56–70 and MOG92–106) develop. Autoreactivity is initiated in part by the in vivo processing of myelin debris and subsequent presentation of myelin epitopes by CNS-resident APCs34. CNS APCs harvested before any signs of demyelination and disease (<40 days after infection) present viral peptides, but not myelin peptides34. However, by 90 days post-infection, microglia and macrophages isolated from the spinal cords of diseased mice endogenously present both viral and myelin epitopes to T cell lines and hybridomas34. Borrow et al. also showed that DTH responses to various myelin epitopes were activated during ongoing TMEV-IDD35. Significantly, induction of tolerance to multiple encephalitogenic myelin epitopes, using the MP-4 fusion protein in SJL mice with ongoing TMEV-IDD, attenuated disease progression and resulted in significantly less demyelination and decreased inflammatory cell infiltration in the CNS36. These results support the hypothesis that tissue damage initiated by virus-specific T cells results in presentation of self antigens and activation of autoreactive T cells in the inflammatory CNS environment, indicating a pathological role for epitope spreading in virus-induced autoimmune disease.
After a microbial infection, activated microbe-specific TH1 (mTH1) cells migrate to the infected organ. A | Molecular mimicry describes the activation of crossreactive TH1 cells that recognize both the microbial epitope (mTH1) and the self epitope (sTH1) (a). Activation of the crossreactive T cells results in the release of cytokines and chemokines (b) that recruit and activate monocytes and macrophages, which mediate self-tissue damage (c). The subsequent release of self-tissue antigens and their uptake by APCs perpetuates the autoimmune disease (d). B | Epitope spreading involves a persistent microbial infection (a) that causes the activation of microorganism-specific TH1 cells (b,c), which mediate self-tissue damage (d). This results in the release of self peptides (e), which are engulfed by APCs and presented to self-reactive TH1 cells (f). Continual damage and release of self peptides results in the spread of the self-reactive immune response to multiple self-epitopes (f). C | Bystander activation is the nonspecific activation of self-reactive TH1 cells. Activation of microorganism-specific TH1 cells (a,b) leads to inflammation (c,d) and results in the increased infiltration of T cells at the site of infection and the activation of self-reactive TH1 cells by TCR-dependent and -independent mechanisms (e) Self-reactive T cells activated in this manner mediate self-tissue damage and perpetuate the autoimmune response (f). D | Cryptic antigen model describing the initiation of autoimmunity by differential processing of self peptides. Following microbial infection (a) IFN-γ is secreted by both activated microbe-specific TH1 cells (b,c) and microbe-infected tissue cells (d). This activates APCs (e) and can lead to APC engulfing self-antigens (f). Cytokine activation of APCs can induce increased protease production and different processing of captured self-antigens, resulting in presentation of cryptic epitopes. The presentation of these cryptic epitopes can activate self-reactive TH1 cells (g), leading to self-tissue destruction (h,i). APC, antigen-presenting cell; MHC II, major histocompatibility complex class II; TCR, T-cell receptor. Modified with permission from Ref. 30.
NOD mouse model of type 1 diabetes. Type 1 diabetes is characterized by a chronic autoimmune response against islet β-cells, which begins early in life. Clinical diabetes, which is the result of the subsequent loss of these cells and their ability to produce insulin, occurs several years later37. INSULITIS — and subsequently diabetes — develops spontaneously in the non-obese diabetic (NOD) mouse and is thought to be primarily dependent on CD4+ TH1 responses. Much work has been done to characterize the specificity of T-cell responses in NOD mice as diabetes develops38,39,40,41,42,43,44. The 45-kd isoform of glutamic acid decarboxylase (GAD45) is considered by many (although not all45) investigators to be the initial target of CD4+ T-cell autoimmunity in this model of diabetes and early tolerance to this response has been shown to block epitope spreading and disease39.
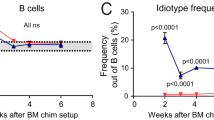
Recent work in human diabetes has focused mainly on humoral responses. Bonifacio et al. examined serum antibodies to insulin, GAD and protein tyrosine phosphatase (islet antigen 2, IA-2) in offspring of diabetic parents at various times, starting at birth. Two distinct autoimmune profiles were observed: a rapid disease onset at the first appearance of an autoantibody response and a slower epitope spreading stage with a later onset of disease. The early response in both subsets (at ∼ 2–3 yr of age) was typically immunoglobulin G1 (IgG1) and most commonly to insulin. IgG1 antibodies to GAD and IA-2 often appeared simultaneously or soon after 2–3 yr of age. In the group with slower disease onset, these initial responses declined (due to antigen-specific regulation) and responses to other antigens appeared46. These investigators also examined epitope spreading, specifically in the anti-GAD antibody response, from birth to disease onset in offspring of diabetic parents. The initial response usually involved anti-GAD64 residues 96–444 and epitope spreading was evident in most offspring47. GAD-specific epitope spreading was also seen in another large study group of diabetic patients48.
Interestingly, pancreas graft rejection in diabetic recipients (under generalized immune suppression) was associated with increased or sustained high levels of humoral islet autoimmunity and with epitope spreading, but not with the levels of GAD- or IA-2-specific serum antibody seen before the allotransplantation49. This implies that recurrent autoimmunity, along with epitope spreading, leads to transplant rejection in diabetic patients.
Models of myasthenia gravis. Myasthenia gravis is characterized by the presence of anti-acetylcholine receptor (AChR) antibodies, which leads to a decreased number of AChRs at the neuromuscular junction, impaired neuromuscular transmission and muscle weakness. Experimental autoimmune myasthenia gravis (EAMG) can be induced in animals by immunization with AChR, leading to AChR-specific T-cell responses and antibody production50. In rabbits, after induction of disease by immunization with three human extracellular peptides, serum antibodies to native AChR are present and bind strongly to rabbit, rather than to human, AChR50,51. This suggests that endogenous presentation of rabbit AChR — which has recently been reported to be mediated by myoblasts52 — during the initial anti-human AChR immune response leads to epitope spreading.
In another model of EAMG, in which C57BL/6 mice are immunized with AChR, anti-CTLA-4 antibody treatment resulted in severe EAMG — which had a rapid onset — enhanced T-cell responses to AChR and increased anti-AChR-antibody production. Anti-CTLA-4 antibody is thought to block a downregulatory signal and therefore increase any ongoing T-cell response. Interestingly, mice immunized with the immunodominant peptide α(146–162) (an extracellular sequence of the AchR) and treated with anti-CTLA-4 showed symptoms of clinical EAMG. Diversification of the autoantibody repertoire and enhanced T-cell proliferation against not only the immunizing α(146–162) peptide, but also other subdominant epitopes, was also evident. Control mice did not show any signs of clinical disease, indicating that treatment with anti-CTLA-4 antibody augmented the initial α(146–162)-specific immune response and led to epitope spreading in both the T- and B-cell components of this pathological autoimmune response53.
Human myasthenia gravis — both early and late onset — is a complex disease that is often characterized by thymic pathologies such as hyperplasia, atrophy or thymoma. Several studies have suggested heterogeneity of T-cell responses against epitopes on the α-, γ- and δ-subunits of AChR; however, much work remains to be done50. In addition to T-cell and antibody epitopes on AChR, antibodies against striated muscle antigens such as titin are characteristic of generalized myasthenia gravis54. This suggests that the immune response in myasthenia gravis is not focused on a dominant epitope. However, studies in patients with the disease in which responses are monitored over time will be necessary to determine whether there is evidence of epitope spreading.
Models of arthritis. Arthritis is an inflammatory disease of the joint synovium. T-cell reactivity towards various synovium- or cartilage-associated antigens has been reported, along with reactivity against microbial and self HEAT-SHOCK PROTEINS (HSPs), which are upregulated by cells under stress and released by necrotic cell death. Adjuvant arthritis, a model of rheumatoid arthritis55,56, is induced in the Lewis rat by injection of COMPLETE FREUND'S ADJUVANT, which contains heat-killed Mycobacterium tuberculosis. There is evidence to suggest that epitope spreading has a role in the pathogenesis of adjuvant arthritis. Moudgil et al. found that the initial T-cell response towards the 65-kDa HSP of M. tuberculosis was focused on epitopes in the middle of this protein, with some reactivity near the N-terminus. By 8–10 weeks after disease onset, reactivity to peptides towards the C-terminus of Mycobacterial hsp65 was evident, and tolerance induced by pretreatment with these C-terminal peptides in synthetic adjuvant blocked arthritis induction57,58. Epitope spreading in this scenario may be secondary to tissue damage, as the spread epitopes represent conserved sequences shared with rat Hsp60. Therefore, epitope spreading might have a protective outcome in this setting. Similarly, synovial T cells taken just before disease remission from patients with juvenile chronic arthritis or rheumatoid arthritis show enhanced responses to self Hsp65 (Ref. 59) and are a good indicator of a favourable prognosis60,61. Further evidence of epitope spreading in rheumatoid arthritis comes from a study by Alam et al., who sequenced more than 650 T-cell receptor (TCR) Vβ D–J junctional regions from synovial and peripheral blood mononuclear cells of two patients with rheumatoid arthritis. Their results indicate that a dynamic TCR selection process takes place during disease progression62.
Epitope spreading in organ allograft rejection
Acute transplant rejection is thought to be the result of direct cytotoxic T lymphocyte (CTL) recognition of MHC class I molecules expressed on donor APCs, because elimination of passenger dendritic cells from the organ substantially reduces transplant rejection. By contrast, indirect helper CD4+ T-cell recognition of recipient MHC class II molecules plus alloantigenic peptide (transplanted tissue processed and presented by host APCs) is most likely to be responsible for chronic rejection63. In human studies, onset of acute rejection in heart transplant recipients was shown to correlate with T-cell responses to a single dominant epitope on one alloantigen64,65. However, in allograft recipients with recurring episodes of rejection or in patients in which chronic rejection was at its onset, recipient T-cell reactivity could spread to other epitopes within the allogeneic MHC molecule, as well as to other alloantigens expressed by graft tissue. In a recent study, recipients of heart allografts were monitored for reactivity against donor human leukocyte antigen (HLA)-DR peptides before and up to 36 months after transplantation64. In patients who received a doubly mismatched transplant (HLA-DR disparity at both loci), chronic rejection was significantly more likely when intermolecular epitope spreading occurred than if reactivity was directed only to the initially targeted HLA-DR molecule65.
Implications for immunotherapy
Substantial evidence from studies of numerous animal models and of various human diseases supports the hypothesis that tissue damage, regardless of the initiating event, can lead to epitope spreading, which can then contribute to ongoing disease. Chronic or persistent infections may trigger, sustain or exacerbate autoimmune disease through epitope spreading via antigen presentation of epitopes released within injured tissue30,66,67. The initial focused immune attack on organ allografts also spreads to include new T- and B-cell reactivity, leading to chronic graft rejection. However, tumour vaccination studies suggest that epitope spreading may increase the efficacy of vaccination protocols.
The immune response therefore appears to be extremely dynamic, with a constantly changing focus. Although the hierarchy and functional significance of responses to spread epitopes can be characterized in defined animal models of immune-mediated disease, gathering this knowledge in human disease is difficult.
Treatment of autoimmunity and transplant rejection. What implications do the phenomena of epitope spreading have for the future of antigen-specific immunotherapies? Currently, it would be difficult to define the pattern of epitope spreading in a chronic human autoimmune disease because the initiating epitope specificity is not known and the epitope dominance and hierarchy of immune responses to multiple tissue antigens would vary depending on the individual's HLA genotype. Therefore, the use of peptide-specific tolerance to treat chronic autoimmune diseases in humans may not be practical at this time. However, as shown in the relapsing EAE models discussed previously, it is theoretically possible to achieve long-term amelioration of autoimmune tissue destruction by inducing peptide-specific tolerance to endogenous tissue epitopes in mice with ongoing disease10. In addition, using an animal model of myasthenia gravis, Xu et al. developed a monoclonal antibody that recognizes the T-cell receptor (TCR) of α(100–116) AChR-specific T cells. Treatment with this mAb reversed ongoing EAMG (when given early after disease onset) and reduced serum antibodies, including antibodies to the main immunogenic region, α(61–76), of the AChR in this rat model68. Although these examples show that, in some disease models, peptide-specific treatments can ameliorate the ongoing disease, direct translation to treatment of human disease is currently difficult.
Another mechanism by which peptide-specific tolerance may result in long-lasting disease inhibition, despite epitope spreading, is via bystander suppression. Treatment of mice to induce TH2-directed immune deviation before or shortly after priming for disease, using therapies induced by self peptide administration by intravenous, oral or nasal routes69,70,71 or by altered peptide ligands (APLs)72, has been shown to inhibit induction of EAE by other epitopes. However, therapy in all of these studies was started before the onset of clinical disease and therefore induced a pre-established anti-inflammatory TH2/regulatory environment. There is a surprising lack of reports in which bystander suppression is used to treat established disease in animal models of autoimmunity, so the efficacy of this approach in the light of ongoing chronic inflammation is not known. As a cautionary note, a recent clinical trial in multiple sclerosis that employed an APL of the HLA-DR2-restricted MBP83–99 epitope led to disease exacerbations in a significant number of patients, in spite of evidence that TH2 responses had been induced73. This may indicate that TH2 cells can contribute to organ-specific autoimmunity in a pre-existing inflammatory setting in which the blood–tissue barrier is compromised. Autoreactive TH2 cells have been shown to be capable of mediating diabetes74 and CNS demyelination75 when transferred to immunodeficient recipients.
As discussed above, our group and others have shown that short-term blockade of either the CD28–CD80/86 or CD40–CD154 co-stimulatory pathways in animals with established relapsing EAE specifically inhibits the initiation of responses to spread epitopes, resulting in long-term protection from disease progression. Short-term co-stimulation blockade, therefore, has the net effect of inducing antigen-specific tolerance, in that these reagents specifically target ongoing T-cell activation (epitope spreading), but only short-term treatment is required.
We have focused primarily on epitope spreading as a mechanism involved in magnification of pathological immune responses. It is likely, however, that epitope spreading is an intrinsic part of an immune reaction, both in magnifying the initial attack and in its subsequent downregulation. Therefore, initiation of TH2 responses via epitope spreading may be an important intrinsic immunoregulatory mechanism in TH1-initiated diseases, geared to limit tissue destruction and promote re-establishment of tissue-specific immune tolerance. Interestingly, in the NOD model of type 1 diabetes, early induction of a TH2 (anti-inflammatory) response to one specific β-cell autoantigen (βCAA), by neonatal priming in incomplete freunds adjuvant, accelerated epitope spreading of TH2 responses to other βCAAs. This spreading of TH2 autoimmunity resulted in active tolerance and reduced disease incidence42,44. Early treatment with any one of several different βCAAs prevents the development of diabetes in the NOD mice, presumably through TH2-mediated epitope spreading leading to the production of anti-inflammatory cytokines. Although the efficiency of this treatment in NOD mice declines when initiated at a later stage in the disease progression, the hope remains that early treatment of human diabetes might lead to therapeutic epitope spreading and disease reduction.
Alloantigen-specific tolerance studies also provide evidence that epitope spreading may be important for immunoregulation. A study examining skin-graft tolerance after donor-specific transfusions found that tolerance induced by transfusions mismatched at one MHC class-I locus actually spread to skin transplants that were mismatched at two MHC-class-I loci or at one MHC-class-I locus plus multiple minor histocompatibility antigens76. This data was interpreted to be the result of epitope spreading of tolerance, but it might involve INFECTIOUS TOLERANCE mediated by CD4+ regulatory T cells77.
Implications for tumour and microbial vaccination. Epitope spreading has also been shown to be involved in the magnification of beneficial (infection and cancer) immune responses. For example, El-Shami et al. have described epitope spreading after ovalbumin (OVA)257–264 peptide immunization plus EG.70VA (thymoma cell line of C57BL/6 transfected with the cDNA of chicken OVA) challenge in C57BL/6 mice78. Injection of EG.7OVA alone results in tumour growth and a CTL response restricted to the immunodominant OVA257–264 epitope. Mice immunized with peptide-pulsed irradiated cells to induce an OVA257–264-specific CTL response and later challenged with a lethal dose of live EG.7OVA tumour cells were completely protected. In addition to OVA257–264, CTL responses in these mice targeted additional OVA peptides (intramolecular epitope spreading) and EL4 cells (intermolecular epitope spreading). Mice that underwent epitope spreading as a result of OVA257–264 vaccination and EG.7OVA-tumour challenge were protected when challenged with live EL4 tumour cells (no OVA antigen present), indicating that the intermolecular epitope spreading induced during the vaccination process was protective. Similar results have been reported in immunity to P815 tumour cells79.
Two recent studies in human cancer research validate research into peptide-based vaccines and indicate that epitope spreading may play an important role in their effectiveness. ERBB2 (HER-2/neu) is a self antigen that is overexpressed in 15–30% of human adenocarcinomas. Patients with ERBB2-overexpressing breast or ovarian tumours received ERBB2 peptides inoculated together with granulocyte–macrophage colony-stimulating factor (GM-CSF), which has been shown in rats to elicit CD4+ T-cell responses to the intact protein. Before vaccination, these patients had no ERBB2-specific responses80. After vaccination with specific peptides, patients acquired immune responses not only to ERBB2 peptide but also to peptides not included in the vaccine (epitope spreading). In another study of breast/ovarian cancer, patients were injected with autologous dendritic cells pulsed with ERBB2- or mucin-1-derived peptides. Data from several patients in this study indicate that immunization with a single tumour antigen may induce CTL reactivity towards several tumour antigens (that is, epitope spreading) in vivo81.
These results indicate that epitope spreading may increase the efficiency of protein vaccination. Although the data described here were obtained from tumour immune responses, the concept may be applicable to microbial vaccination.
Concluding remarks
The immune response is remarkably complex and strives to maintain a balance between pro- and anti-inflammatory responses. Understanding the temporal dynamics of sequential immune responses to newly arising specificities and how these affect disease pathology and regulation remains an important area of study in autoimmunity, transplantation and vaccination. The immune response consists of both the initial magnification phase — which can be either deleterious, as in autoimmune disease, or beneficial, as in vaccinations or infectious disease — and a later downregulatory phase to return the immune system to homeostasis. Epitope spreading may be an important component of both phases. Knowledge of the pattern of epitope spreading in human autoimmune disease or transplant rejection could be used to design antigen-specific therapies that block ongoing tissue destruction or organ rejection, respectively. Alternatively, therapies could be designed to enhance the natural downregulatory mechanisms. For example, magnification of TH2 responses via epitope spreading could be used to suppress pathogenic TH1 responses for protection against the development of diabetes, as discussed above.
As discussed, identifying the hierarchy and functional significance of epitopes involved in human autoimmune diseases is difficult at present. Technical limitations aside, short-term co-stimulatory blockade (CD28 or CD154) in animal models has been shown to affect long-term antigen-specific regulation of responses to spread epitopes. It is also important to note that epitope spreading during magnification of immune responses is not always pathological, but can be beneficial. For example, the use of peptide vaccines for tumour or microbial vaccination may be more efficient than once thought, given that responses to the initial peptide may be followed by responses to additional tumour or microbial peptides via epitope spreading, enhancing the efficacy of protection or therapy. Reagents like anti-CTLA-4, which lower the threshold of T-cell activation and enhance the magnification of T-cell responses, thereby accelerating epitope spreading, may improve the efficacy of tumour or microbial peptide vaccines15,82,83.
As described in this review, attempts to manipulate the pro-inflammatory/anti-inflammatory balance of the immune system can lead to unexpected consequences. Although the studies discussed here indicate that there are multiple possible therapeutic avenues to explore, a much greater understanding of the regulation of the immune system is required before effective and safe therapies can be applied to human disease.
References
Lehmann, P. V., Forsthuber, T., Miller, A. & Sercarz, E. E. Spreading of T-cell autoimmunity to cryptic determinants of an autoantigen. Nature 358, 155–157 (1992).The first description of epitope spreading in an autoimmune disease.
Lehmann, P. V., Sercarz, E. E., Forsthuber, T., Dayan, C. M. & Gammon, G. Determinant spreading and the dynamics of the autoimmune T-cell repertoire. Immunol. Today 14, 203–208 (1993).
Lehmann, P. V., Targoni, O. S. & Forsthuber, T. G. Shifting T-cell activation thresholds in autoimmunity and determinant spreading. Immunol. Rev. 164, 53–61 (1998).
Steinman, L. Despite epitope spreading in the pathogenesis of autoimmune disease, highly restricted approaches to immune therapy may still succeed [with a hedge on this bet]. J. Autoimmun. 14, 278–282 (2000).
Yu, M., Johnson, J. M. & Tuohy, V. K. A predictable sequential determinant spreading cascade invariably accompanies progression of experimental autoimmune encephalomyelitis: a basis for peptide-specific therapy after onset of clinical disease. J. Exp. Med. 183, 1777–1788 (1996).
Vanderlugt, C. L. et al. The functional significance of epitope spreading and its regulation by co-stimulatory molecules. Immunol. Rev. 164, 63–72 (1998).
Kumar, V. Determinant spreading during experimental autoimmune encephalomyelitis: is it potentiating, protecting or participating in the disease? Immunol. Rev. 164, 73–80 (1998).
Tuohy, V. K. et al. The epitope spreading cascade during progression of experimental autoimmune encephalomyelitis and multiple sclerosis. Immunol. Rev. 164, 93–100 (1998).
McRae, B. L., Vanderlugt, C. L., Dal Canto, M. C. & Miller, S. D. Functional evidence for epitope spreading in the relapsing pathology of experimental autoimmune encephalomyelitis. J. Exp. Med. 182, 75–85 (1995).The first demonstration that epitope spreading has pathological significance in ongoing autoimmunity.
Vanderlugt, C. L. et al. Pathologic role and temporal appearance of newly emerging autoepitopes in relapsing experimental autoimmune encephalomyelitis. J. Immunol. 164, 670–678 (2000).A demonstration that ongoing autoimmunity and epitope spreading can be specifically inhibited by peptide-specific tolerance or blockade of CD80/86–CD28 co-stimulation.
Kennedy, M. K. et al. Inhibition of murine relapsing experimental autoimmune encephalomyelitis by immune tolerance to proteolipid protein and its encephalitogenic peptides. J. Immunol. 144, 909–915 (1990).
Anderson, A. C. et al. High frequency of autoreactive myelin proteolipid protein-specific T cells in the periphery of naive mice: mechanisms of selection of the self-reactive repertoire. J. Exp. Med. 191, 761–770 (2000).
Miller, S. D. et al. Blockade of CD28/B7-1 interaction prevents epitope spreading and clinical relapses of murine EAE. Immunity 3, 739–745 (1995).
Howard, L. M. et al. Mechanisms of immunotherapeutic intervention by anti-CD40L (CD154) antibody in an animal model of multiple sclerosis. J. Clin. Invest. 103, 281–290 (1999).Evidence that blockade of CD40/CD154 co-stimulation can ameliorate ongoing autoimmunity and epitope spreading.
Karandikar, N. J., Eagar, T. A., Vanderlugt, C. L., Bluestone, J. A. & Miller, S. D. CTLA-4 downregulates epitope spreading and mediates remission in autoimmune disease. J. Neuroimmunol. 109, 173–180 (2000).
Karandikar, N. J., Vanderlugt, C. L., Bluestone, J. A. & Miller, S. D. Targeting the B7/CD28:CTLA-4 costimulatory system in CNS autoimmune disease. J. Neuroimmunol. 89, 10–18 (1998).
Tuohy, V. K., Yu, M., Yin, L., Kawczak, J. A. & Kinkel, P. R. Regression and spreading of self-recognition during the development of autoimmune demyelinating disease. J. Autoimmun. 13, 11–20 (1999).
Rudick, R. A. Disease-modifying drugs for relapsing-remitting multiple sclerosis and future directions for multiple sclerosis therapeutics. Arch. Neurol. 56, 1079–1084 (1999).
Arnason, B. G. Immunologic therapy of multiple sclerosis. Annu. Rev. Med. 50, 291–302 (1999).
Tuohy, V. K. et al. Modulation of the IL-10/IL-12 cytokine circuit by interferon-β inhibits the development of epitope spreading and disease progression in murine autoimmune encephalomyelitis. J. Neuroimmunol. 111, 55–63 (2000).
Fiorentino, D. F., Zlotnik, A., Mosman, T. R., Howard, M. H. & O'Garra, A. IL-10 inhibits cytokine production by activated macrophages. J. Immunol. 147, 3815–3822 (1991).
Fiorentino, D. F. et al. IL-10 acts on the antigen-presenting cell to inhibit cytokine production by TH1 cells. J. Immunol. 146, 3444–3451 (1991).
De Waal Malefyt, R., Abrams, J., Bennett, B., Figdor, C. G. & De Vries, J. E. Interleukin 10 (IL-10) inhibits cytokine synthesis by human monocytes: an autoregulatory role of IL-10 produced by monocytes. J. Exp. Med. 174, 1209–1220 (1991).
Ding, L. & Shevach, E. M. IL-10 inhibits mitogen-induced T cell proliferation by selectively inhibiting macrophage costimulatory function. J. Immunol. 148, 3133–3139 (1992).
McFarland, H. I. et al. Determinant spreading associated with demyelination in a nonhuman primate model of multiple sclerosis. J. Immunol. 162, 2384–2390 (1999).
Tuohy, V. K., Yu, M., Weinstock-Guttman, B. & Kinkel, R. P. Diversity and plasticity of self recognition during the development of multiple sclerosis. J. Clin. Invest. 99, 1682–1690 (1997).An initial demonstration of spreading and focusing of responses to PLP epitopes during the progression of multiple sclerosis.
Tuohy, V. K., Yu, M., Yin, L., Kawczak, J. A. & Kinkel, R. P. Spontaneous regression of primary autoreactivity during chronic progression of experimental autoimmune encephalomyelitis and multiple sclerosis. J. Exp. Med. 189, 1033–1042 (1999).
Goebels, N. et al. Repertoire dynamics of autoreactive T cells in multiple sclerosis patients and healthy subjects: epitope spreading versus clonal persistence. Brain 123, 508–518 (2000).
Kurtzke, J. F. Epidemiologic evidence for multiple sclerosis as an infection. Clin. Microbiol. Rev. 6, 382–427 (1993).
Olson, J. K., Croxford, J. L. & Miller, S. D. Virus-induced autoimmunity: potential role of viruses in initiation, perpetuation, and progression of T cell-mediated autoimmune diseases. Viral Immunol. 14, 227–250 (2001).
Karpus, W. J., Pope, J. G., Peterson, J. D., Dal Canto, M. C. & Miller, S. D. Inhibition of Theiler's virus-mediated demyelination by peripheral immune tolerance induction. J. Immunol. 155, 947–957 (1995).
Miller, S. D. et al. Persistent infection with Theiler's virus leads to CNS autoimmunity via epitope spreading. Nature Med. 3, 1133–1136 (1997).The first description that a persistent virus infection can lead to autoimmunity via epitope spreading.
Katz-Levy, Y. et al. Temporal development of autoreactive TH1 responses and endogenous antigen presentation of self myelin epitopes by CNS-resident APCs in Theiler's virus-infected mice. J. Immunol. 165, 5304–5314 (2000).
Katz-Levy, Y. et al. Endogenous presentation of self myelin epitopes by CNS-resident APCs in Theiler's virus-infected mice. J. Clin. Invest. 104, 599–610 (1999).Evidence of endogenous presentation of self epitopes by resident APCs in the target tissue of the disease.
Borrow, P. et al. Investigation of the role of delayed-type-hypersensitivity responses to myelin in the pathogenesis of Theiler's virus-induced demyelinating disease. Immunology 93, 478–484 (1998).
Neville, K. L., Padilla, J. & Miller, S. D. Myelin-specific tolerance attenuates the progression of a virus-induced demyelinating disease: implications for the treatment of MS. J. Neuroimmunol. (In the press).
Eisenbarth, G. S. Type I diabetes mellitus. A chronic autoimmune disease. N. Engl. J. Med. 314, 1360–1368 (1986).
Delovitch, T. L. & Singh, B. The nonobese diabetic mouse as a model of autoimmune diabetes: immune dysregulation gets the NOD. Immunity 7, 727–738 (1997).
Kaufman, D. L. et al. Spontaneous loss of T cell tolerance to glutamic acid decarboxylase in murine insulin-dependent diabetes. Nature 366, 69–72 (1993).
Zechel, M. A., Elliott, J. F., Atkinson, M. A. & Singh, B. Characterization of novel T-cell epitopes on 65 kDa and 67 kDa glutamic acid decarboxylase relevant in autoimmune responses in NOD mice. J. Autoimmun. 11, 83–95 (1998).
Zechel, M. A., Chaturvedi, P. & Singh, B. Characterization of immunodominant peptide determinants of IDDM-associated autoantigens in the NOD mouse. Res. Immunol. 148, 338–348 (1997).
Tian, J., Lehmann, P. V. & Kaufman, D. L. Determinant spreading of T helper cell 2 (TH2) responses to pancreatic islet autoantigens. J. Exp. Med. 186, 2039–2043 (1997).Evidence of protective epitope spreading.
Zechel, M. A., Krawetz, M. D. & Singh, B. Epitope dominance: evidence for reciprocal determinant spreading to glutamic acid decarboxylase in non-obese diabetic mice. Immunol. Rev. 164, 111–118 (1998).
Tian, J. et al. Infectious TH1 and TH2 autoimmunity in diabetes-prone mice. Immunol. Rev. 164, 119–127 (1998).
Durinovic-Bello, I. Autoimmune diabetes: the role of T cells, MHC molecules and autoantigens. Autoimmunity 27, 159–177 (1998).
Bonifacio, E., Scirpoli, M., Kredel, K., Fuchtenbusch, M. & Ziegler, A. G. Early autoantibody responses in prediabetes are IgG1 dominated and suggest antigen-specific regulation. J. Immunol. 163, 525–532 (1999).
Bonifacio, E., Lampasona, V., Bernasconi, L. & Ziegler, A. G. Maturation of the humoral autoimmune response to epitopes of GAD in preclinical childhood type 1 diabetes. Diabetes 49, 202–208 (2000).
Sohnlein, P. et al. Epitope spreading and a varying but not disease-specific GAD65 antibody response in type I diabetes. The Childhood Diabetes in Finland Study Group. Diabetologia 43, 210–217 (2000).
Braghi, S. et al. Modulation of humoral islet autoimmunity by pancreas allotransplantation influences allograft outcome in patients with type 1 diabetes. Diabetes 49, 218–224 (2000).
Vincent, A. et al. Determinant spreading and immune responses to acetylcholine receptors in myasthenia gravis. Immunol. Rev. 164, 157–168 (1998).
Vincent, A., Jacobson, L. & Shillito, P. Response to human acetylcholine receptor α 138–199: determinant spreading initiates autoimmunity to self-antigen in rabbits. Immunol. Lett. 39, 269–275 (1994).
Curnow, J., Corlett, L., Willcox, N. & Vincent, A. Presentation by myoblasts of an epitope from endogenous acetylcholine receptor indicates a potential role in the spreading of the immune response. J. Neuroimmunol. 115, 127–134 (2001).
Wang, H. B. et al. Anti-CTLA-4 antibody treatment triggers determinant spreading and enhances murine myasthenia gravis. J. Immunol. 166, 6430–6436 (2001).
Yamamoto, A. M. et al. Anti-titin antibodies in myasthenia gravis: tight association with thymoma and heterogeneity of nonthymoma patients. Arch. Neurol. 58, 885–890 (2001).
Van Eden, W. et al. Heat-shock protein T-cell epitopes trigger a spreading regulatory control in a diversified arthritogenic T-cell response. Immunol. Rev. 164, 169–174 (1998).
Sonderstrup, G. & McDevitt, H. Identification of autoantigen epitopes in MHC class II transgenic mice. Immunol. Rev. 164, 129–138 (1998).
Moudgil, K. D. et al. Diversification of T cell responses to carboxy-terminal determinants within the 65-kD heat-shock protein is involved in regulation of autoimmune arthritis. J. Exp. Med. 185, 1307–1316 (1997).
Moudgil, K. D. Diversification of response to hsp65 during the course of autoimmune arthritis is regulatory rather than pathogenic. Immunol. Rev. 164, 175–184 (1998).
Prakken, A. B. et al. Autoreactivity to human heat-shock protein 60 predicts disease remission in oligoarticular juvenile rheumatoid arthritis. Arthritis Rheum. 39, 1826–1832 (1996).
Prakken, A. B. et al. T-cell reactivity to human HSP60 in oligo-articular juvenile chronic arthritis is associated with a favorable prognosis and the generation of regulatory cytokines in the inflamed joint. Immunol. Lett. 57, 139–142 (1997).
deGraeff-Meeder, E. R. et al. Juvenile chronic arthritis: T cell reactivity to human HSP60 in patients with a favorable course of arthritis. J. Clin. Invest. 95, 934–940 (1995).
Alam, A. et al. Persistence of dominant T cell clones in synovial tissues during rheumatoid arthritis. J. Immunol. 156, 3480–3485 (1996).
Bradley, J. A. Indirect T cell recognition in allograft rejection. Int. Rev. Immunol. 13, 245–255 (1996).
Suciu-Foca, N., Harris, P. E. & Cortesini, R. Intramolecular and intermolecular spreading during the course of organ allograft rejection. Immunol. Rev. 164, 241–246 (1998).
Ciubotariu, R. et al. Persistent allopeptide reactivity and epitope spreading in chronic rejection of organ allografts. J. Clin. Invest 101, 398–405 (1998).Evidence of epitope spreading in allograft rejection.
Di Rosa, F. & Barnaba, V. Persisting viruses and chronic inflammation: understanding their relation to autoimmunity. Immunol. Rev. 164, 17–27 (1998).
Dorries, R. The role of T-cell-mediated mechanisms in virus infections of the nervous system. Curr. Top. Microbiol. Immunol. 253, 219–245 (2001).
Xu, L., Villain, M., Galin, F. S., Araga, S. & Blalock, J. E. Prevention and reversal of experimental autoimmune myasthenia gravis by a monoclonal antibody against acetylcholine receptor-specific T cells. Cell Immunol. 208, 107–114 (2001).
Leadbetter, E. A. et al. Experimental autoimmune encephalomyelitis induced with a combination of myelin basic protein and myelin oligodendrocyte glycoprotein is ameliorated by administration of a single myelin basic protein peptide. J. Immunol. 161, 504–512 (1998).
Al-Sabbagh, A., Nelson, P. A., Akselband, Y., Sobel, R. A. & Weiner, H. L. Antigen-driven peripheral immune tolerance: suppression of experimental autoimmmune encephalomyelitis and collagen-induced arthritis by aerosol administration of myelin basic protein or type II collagen. Cell. Immunol. 171, 111–119 (1996).
Anderton, S. M. & Wraith, D. C. Hierarchy in the ability of T cell epitopes to induce peripheral tolerance to antigens from myelin. Eur. J. Immunol. 28, 1251–1261 (1998).
Nicholson, L. B., Murtaza, A., Hafler, B. P., Sette, A. & Kuchroo, V. K. A T cell receptor antagonist peptide induces T cells that mediate bystander suppression and prevent autoimmune encephalomyelitis induced with multiple myelin antigens. Proc. Natl Acad. Sci. USA 94, 9279–9284 (1997).
Bielekova, B. et al. Encephalitogenic potential of the myelin basic protein peptide (amino acids 83–99) in multiple sclerosis: results of a phase II clinical trial with an altered peptide ligand. Nature Med. 6, 1167–1175 (2000).
Pakala, S. V., Kurrer, M. O. & Katz, J. D. T helper 2 (TH2) T cells induce acute pancreatitis and diabetes in immune-compromised nonobese diabetic (NOD) mice. J. Exp. Med. 186, 299–306 (1997).
Lafaille, J. J. et al. Myelin basic protein-specific T helper 2 (TH2) cells cause experimental autoimmune encephalomyelitis in immunodeficient hosts rather than protect them from the disease. J. Exp. Med. 186, 307–312 (1997).
Yang, L., DuTemple, B., Gorczynski, R. M., Levy, G. & Zhang, L. Evidence for epitope spreading and active suppression in skin graft tolerance after donor-specific transfusion. Transplantation 67, 1404–1410 (1999).
Waldmann, H. & Cobbold, S. Regulating the immune response to transplants: a role for CD4+ regulatory cells? Immunity 14, 399–406 (2001).
el Shami, K. et al. MHC class I-restricted epitope spreading in the context of tumor rejection following vaccination with a single immunodominant CTL epitope. Eur. J. Immunol. 29, 3295–3301 (1999).Evidence of MHC-class-I–restricted epitope spreading in tumour immunity.
Markiewicz, M. A., Fallarino, F., Ashikari, A. & Gajewski, T. F. Epitope spreading upon P815 tumor rejection triggered by vaccination with the single class I MHC-restricted peptide P1A. Int. Immunol. 13, 625–632 (2001).
Disis, M. L., Grabstein, K. H., Sleath, P. R. & Cheever, M. A. Generation of immunity to the HER-2/neu oncogenic protein in patients with breast and ovarian cancer using a peptide-based vaccine. Clin. Cancer Res. 5, 1289–1297 (1999).
Brossart, P. et al. Induction of cytotoxic T-lymphocyte responses in vivo after vaccinations with peptide-pulsed dendritic cells. Blood 96, 3102–3108 (2000).
Leach, D. R., Krummel, M. F. & Allison, J. P. Enhancement of antitumor immunity by CTLA-4 blockade. Science 271, 1734–1736 (1996).
Hurwitz, A. A., Yu, T. F., Leach, D. R. & Allison, J. P. CTLA-4 blockade synergizes with tumor-derived granulocyte–macrophage colony-stimulating factor for treatment of an experimental mammary carcinoma. Proc. Natl Acad. Sci. USA 95, 10067–10071 (1998).
Olson, J. K., Croxford, J. L., Calenoff, M., Dal Canto, M. C. & Miller, S. D. A virus-induced molecular mimicry model of multiple sclerosis. J. Clin. Invest. 108, 311–318 (2001).Evidence that epitope spreading can be initiated after induction of autoimmunity via molecular mimicry.
Mokhtarian, F., Shi, Y., Zhu, P. F. & Grob, D. Immune responses, and autoimmune outcome, during virus infection of the central nervous system. Cell. Immunol. 157, 195–210 (1994).
Mokhtarian, F., Zhang, Z., Shi, Y., Gonzales, E. & Sobel, R. A. Molecular mimicry between a viral peptide and a myelin oligodendrocyte glycoprotein peptide induces autoimmune demyelinating disease in mice. J. Neuroimmunol. 95, 43–54 (1999).
Lawson, C. M. Evidence for mimicry by viral antigens in animal models of autoimmune disease including myocarditis. Cell Mol. Life Sci. 57, 552–560 (2000).
Fairweather, D., Kaya, Z., Shellam, G. R., Lawson, C. M. & Rose, N. R. From infection to autoimmunity. J. Autoimmun. 16, 175–186 (2001).
Horwitz, M. S. et al. Diabetes induced by Coxsackie virus: initiation by bystander damage and not molecular mimicry. Nature Med. 4, 781–786 (1998).
Zhao, Z.-S., Granucci, F., Yeh, L., Schaffer, P. A. & Cantor, H. Molecular mimicry by herpes simplex virus-type 1: Autoimmune disease after viral infection. Science 279, 1344–1347 (1998).
Deshpande, S. P. et al. Herpes simplex virus-induced keratitis: evaluation of the role of molecular mimicry in lesion pathogenesis. J. Virol. 75, 3077–3088 (2001).
Author information
Authors and Affiliations
Corresponding author
Glossary
- CRYPTIC EPITOPE
-
A cryptic epitope is defined as a hidden or sequestered epitope that is processed and presented more efficiently as a result of an inflammatory immune response initiated by either a dominant epitope, as in a response to an infectious agent, or revealed as a result of the diversification of the response secondary to self tissue damage, as in an autoimmune response.
- T HELPER TYPE 1 (TH1)
-
CD4+ T cells have been divided into at least two distinct types. TH1 cells produce IFN-γ, lymphotoxin and TNF-α, and mediate macrophage inflammatory responses such as delayed-type hypersensitivity (DTH). Demyelination in multiple sclerosis models is thought to be due to TH1 cells. TH2 cells produce IL-4, IL-10 and/or TGF-β, and can downregulate TH1 responses.
- INTRAMOLECULAR EPITOPE SPREADING
-
Spreading from one epitope to another on the same molecule, for example, from PLP139–151 to PLP178–191.
- INTERMOLECULAR EPITOPE SPREADING
-
Spreading of the specificity of an immune response from an epitope on one molecule to one on a different molecule is termed intermolecular epitope spreading. An example would be the spread in EAE induced with PLP139–151, an epitope on proteolipid protein, to an epitope on myelin basic protein, such as MBP84–104.
- ISOLATED MONOSYMPTOMATIC DEMYELINATING SYNDROME
-
(IMDS). IMDS is a group of distinct clinical disorders often associated with eventual progression toward clinically definite multiple sclerosis.
- TCR Vβ CDR3 SPECTRATYPING
-
Polymerase chain reaction-based method of identifying pseudoclonal TCR usage by analyzing Vβ family gene usage. In independent reactions, Vβ–Cβ products across the CDR3 region are amplified from cDNA, tagged with a fluorochrome, and resolved on a polyacrylamide gel electrophoresis gel. Expanded pseudoclonal Vβ–Cβ products of a single length are distinguished from other Vβ–Cβ products by size differences introduced at the coding junction.
- INSULITIS
-
Inflammation surrounding the insulin-producing β-cells in the pancreas. Diabetes occurs when β-cells can no longer produce adequate amounts of insulin.
- HEAT-SHOCK PROTEIN
-
Heat-shock proteins are expressed in all cells, including microbes, when they are stressed; for example, when they experience high temperatures. These proteins can then become targeted by an immune response.
- COMPLETE FREUND'S ADJUVANT
-
Used to trigger an immune response to proteins or peptides emulsified in the adjuvant; it consists of freeze-dried Mycobacterium, emulsifying agents and mineral oil.
- INFECTIOUS TOLERANCE
-
Production of anti-inflammatory cytokines (e.g. IL-4, IL-10, TGF-β) by an antigen-specific regulatory T cell, which suppress immune responses to additional epitopes in a non-specific manner.
Rights and permissions
About this article
Cite this article
Vanderlugt, C., Miller, S. Epitope spreading in immune-mediated diseases: implications for immunotherapy. Nat Rev Immunol 2, 85–95 (2002). https://doi.org/10.1038/nri724
Issue Date:
DOI: https://doi.org/10.1038/nri724
This article is cited by
-
Novel Clinical Trials and Approaches in the Management of Glioblastoma
Current Oncology Reports (2024)
-
Possible Role of Dysbiosis of the Gut Microbiome in SLE
Current Rheumatology Reports (2023)
-
Incorporating the Molecular Mimicry of Environmental Antigens into the Causality of Autoimmune Hepatitis
Digestive Diseases and Sciences (2023)
-
Antigen presentation by B cells enables epitope spreading across an MHC barrier
Nature Communications (2023)
-
A case of meningoencephalomyelitis associated with immune-mediated necrotizing myopathy
Neurological Sciences (2022)