Abstract
Background
Recent findings have shown that the neutrophil-to-lymphocyte ratio (NLR) is prognostic for gastrointestinal stromal tumors (GIST). The platelet-to-lymphocyte ratio (PLR) can predict outcome for several other disease sites. This study evaluates the prognostic utility of NLR and PLR for patients with GIST.
Methods
All patients who had undergone surgical resection for primary, localized GIST from 2001 to 2011 were identified from a prospectively maintained database. Recurrence-free survival (RFS) was calculated by the Kaplan–Meier method and compared by the log-rank test. Univariate Cox proportional hazard regression models were used to identify associations with outcome variables.
Results
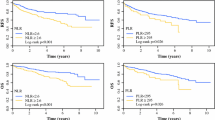
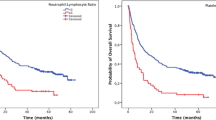
The study included 93 patients. High PLR [≥245; hazard ratio (HR) 3.690; 95 % confidence interval (CI) 1.066–12.821; p = 0.039], neutrophils (HR 1.224; 95 % CI 1.017–1.473; p = 0.033), and platelets (HR 1.005; 95 % CI 1.001–1.009; p = 0.013) were associated with worse RFS. Patients with high PLR had 2- and 5-year RFS of 57 and 57 %, compared with 94 and 84 % for those with low PLR. High NLR (≥2.04) was not associated with reduced RFS (p = 0.214). Whereas more patients in the high PLR group had large tumors (p = 0.047), more patients in the high NLR group had high mitotic rates (p = 0.016) than in the low-ratio cohorts. Adjuvant therapy was given to 41.2 % of the patients with high PLR (p = 0.022). The patients with high PLR/NLR had worse nomogram-predicted RFS than the patients with low PLR/NLR.
Conclusions
High PLR was associated with reduced RFS. The prognostic ability of PLR to predict recurrence suggests that it may play a role in risk-stratification schemes used to determine which patients will benefit from adjuvant therapy.


Similar content being viewed by others
References
Connolly EM, Gaffney E, Reynolds JV. Gastrointestinal stromal tumours. Br J Surg. 2003;90:1178–86.
Miettinen M, Sarlomo-Rikala M, Lasota J. Gastrointestinal stromal tumours. Ann Chir Gynaecol. 1998;87:278–81.
Hasegawa T, Matsuno Y, Shimoda T, Hirohashi S. Gastrointestinal stromal tumor: consistent CD117 immunostaining for diagnosis, and prognostic classification based on tumor size and MIB-1 grade. Hum Pathol. 2002;33:669–76.
Hirota S, Isozaki K, Moriyama Y, et al. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science. 1998;279:577–80.
Heinrich MC, Corless CL, Duensing A, et al. PDGFRA activating mutations in gastrointestinal stromal tumors. Science. 2003;299:708–10.
Blay JY, von Mehren M, Blackstein ME. Perspective on updated treatment guidelines for patients with gastrointestinal stromal tumors. Cancer. 2010;116:5126–37.
Tran T, Davila JA, El-Serag HB. The epidemiology of malignant gastrointestinal stromal tumors: an analysis of 1,458 cases from 1992 to 2000. Am J Gastroenterol. 2005;100:162–8.
Nilsson B, Bumming P, Meis-Kindblom JM, et al. Gastrointestinal stromal tumors: the incidence, prevalence, clinical course, and prognostication in the preimatinib mesylate era: a population-based study in western Sweden. Cancer. 2005;103:821–9.
Di Matteo G, Pescarmona E, Peparini N, et al. Histopathological features and clinical course of the gastrointestinal stromal tumors. Hepatogastroenterology. 2002;49:1013–6.
Tornoczky T, Kalman E, Hegedus G, et al. High mitotic index associated with poor prognosis in gastrointestinal autonomic nerve tumour. Histopathology. 1999;35:121–8.
Wang X, Mori I, Tang W, et al. Helpful parameter for malignant potential of gastrointestinal stromal tumors (GIST). Jpn J Clin Oncol. 2002;32:347–51.
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454:436–44.
Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140:883–99.
Guthrie GJ, Charles KA, Roxburgh CS, Horgan PG, McMillan DC, Clarke SJ. The systemic inflammation-based neutrophil-lymphocyte ratio: experience in patients with cancer. Crit Rev Oncol Hematol. 2013;88:218–30.
Perez DR, Baser RE, Cavnar MJ, et al. Blood neutrophil-to-lymphocyte ratio is prognostic in gastrointestinal stromal tumor. Ann Surg Oncol. 2013;20:593–9.
Smith RA, Bosonnet L, Raraty M, Sutton R, Neoptolemos JP, Campbell F, Ghaneh P. Preoperative platelet–lymphocyte ratio is an independent significant prognostic marker in resected pancreatic ductal adenocarcinoma. Am J Surg. 2009;197:466–72.
Asher V, Lee J, Innamaa A, Bali A. Preoperative platelet–lymphocyte ratio as an independent prognostic marker in ovarian cancer. Clin Transl Oncol. 2011;13:499–503.
Kwon HC, Kim SH, Oh SY, et al. Clinical significance of preoperative neutrophil–lymphocyte versus platelet–lymphocyte ratio in patients with operable colorectal cancer. Biomarkers. 2012;17:216–22.
Feng JF, Huang Y, Zhao Q, Chen QX. Clinical significance of preoperative neutrophil–lymphocyte ratio versus platelet–lymphocyte ratio in patients with small cell carcinoma of the esophagus. Sci World J. 2013;2013:504365.
Wang D, Yang JX, Cao DY, et al. Preoperative neutrophil–lymphocyte and platelet–lymphocyte ratios as independent predictors of cervical stromal involvement in surgically treated endometrioid adenocarcinoma. Onco Targets Ther. 2013;6:211–6.
Fletcher CD, Berman JJ, Corless C, et al. Diagnosis of gastrointestinal stromal tumors: a consensus approach. Hum Pathol. 2002;33:459–65.
Joensuu H. Risk stratification of patients diagnosed with gastrointestinal stromal tumor. Hum Pathol. 2008;39:1411–9.
Gold JS, Gonen M, Gutierrez A, et al. Development and validation of a prognostic nomogram for recurrence-free survival after complete surgical resection of localised primary gastrointestinal stromal tumour: a retrospective analysis. Lancet Oncol. 2009;10:1045–52.
Ong SL, Garcea G, Thomasset SC, et al. Surrogate markers of resectability in patients undergoing exploration of potentially resectable pancreatic adenocarcinoma. J Gastrointest Surg. 2008;12:1068–73.
Miettinen M, Majidi M, Lasota J. Pathology and diagnostic criteria of gastrointestinal stromal tumors (GISTs): a review. Eur J Cancer. 2002;38(Suppl 5):S39–51.
Miettinen M, Lasota J. Gastrointestinal stromal tumors—definition, clinical, histological, immunohistochemical, and molecular genetic features and differential diagnosis. Virchows Arch. 2001;438:1–12.
Racz JM, Brar SS, Cleghorn MC, et al. The accuracy of three predictive models in the evaluation of recurrence rates for gastrointestinal stromal tumours. J Surg Oncol. 2014 (in press).
Proctor MJ, Morrison DS, Talwar D, et al. A comparison of inflammation-based prognostic scores in patients with cancer: a Glasgow Inflammation Outcome Study. Eur J Cancer. 2011;47:2633–41.
Raungkaewmanee S, Tangjitgamol S, Manusirivithaya S, Srijaipracharoen S, Thavaramara T. Platelet-to-lymphocyte ratio as a prognostic factor for epithelial ovarian cancer. J Gynecol Oncol. 2012;23:265–73.
Sakka N, Smith RA, Whelan P, et al. A preoperative prognostic score for resected pancreatic and periampullary neuroendocrine tumours. Pancreatology. 2009;9:670–6.
Smith RA, Ghaneh P, Sutton R, Raraty M, Campbell F, Neoptolemos JP. Prognosis of resected ampullary adenocarcinoma by preoperative serum CA19-9 levels and platelet–lymphocyte ratio. J Gastrointest Surg. 2008;12:1422–8.
Bhatti I, Peacock O, Lloyd G, Larvin M, Hall RI. Preoperative hematologic markers as independent predictors of prognosis in resected pancreatic ductal adenocarcinoma: neutrophil–lymphocyte versus platelet–lymphocyte ratio. Am J Surg. 2010;200:197–203.
Buergy D, Wenz F, Groden C, Brockmann MA. Tumor–platelet interaction in solid tumors. Int J Cancer. 2012;130:2747–60.
Goubran HA, Burnouf T, Radosevic M, El-Ekiaby M. The platelet–cancer loop. Eur J Intern Med. 2013;24:393–400.
Kinoshita A, Onoda H, Imai N, et al. Comparison of the prognostic value of inflammation-based prognostic scores in patients with hepatocellular carcinoma. Br J Cancer. 2012;107:988–93.
Leitch EF, Chakrabarti M, Crozier JE, McKee RF, Anderson JH, Horgan PG, McMillan DC. Comparison of the prognostic value of selected markers of the systemic inflammatory response in patients with colorectal cancer. Br J Cancer. 2007;97:1266–70.
Gondo T, Nakashima J, Ohno Y, et al. Prognostic value of neutrophil-to-lymphocyte ratio and establishment of novel preoperative risk stratification model in bladder cancer patients treated with radical cystectomy. Urology. 2012;79:1085–91.
Ishizuka M, Nagata H, Takagi K, Iwasaki Y, Kubota K. Combination of platelet count and neutrophil-to-lymphocyte ratio is a useful predictor of postoperative survival in patients with colorectal cancer. Br J Cancer. 2013;109:401–7.
Disclosure
The authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Racz, J.M., Cleghorn, M.C., Jimenez, M.C. et al. Predictive Ability of Blood Neutrophil-to-Lymphocyte and Platelet-to-Lymphocyte Ratios in Gastrointestinal Stromal Tumors. Ann Surg Oncol 22, 2343–2350 (2015). https://doi.org/10.1245/s10434-014-4265-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-4265-6